Video Link: https://vimeo.com/293632049
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Late last year, an article was published by the Journal of the American Medical Association that suggested Testosterone Restoration was associated with an  increased risk of stroke, heart attack, and general mortality in males suffering from Low-T.
increased risk of stroke, heart attack, and general mortality in males suffering from Low-T.
Mainly as a result of this study, the FDA now requires that all Testosterone Therapy Manufacturers clearly note these potential risks associated with therapy on every dose of Testosterone Treatment.
There's no reason to have issues with the FDA in this case because that's a reasonable step to take, but the study which precipitated this change in Testosterone labeling was highly flawed, and an example of media entities taking surveys in a vacuum and treating them as the definitive word on a particular treatment.
We might want to be skeptical or "trust but verify" by looking at other studies, because according to some studies, 1/3rd of men who suffer from heart attacks have low testosterone levels.
JAMA Testosterone Study Flawed
In reality, this Testosterone Study is highly flawed, at least when considered as a potential indictment against Low-T Treatment for men suffering from Testosterone Deficiency and Andropause.
There's even the risk that this study could lead patients who could seriously benefit from this form of Hormone Therapy Treatment to avoid life-changing treatment because of the unwarranted fears suggested by this study.
In fact, many medical professionals say the validity of this study about Testosterone Therapy prescribed and administered with care and caution is effectively nil.
Though we should still be cautious, and not dismiss the risks which are being claimed.
Over the past decade, there have been some studies providing strong evidence that Low-T Treatment with Bio-Identical Testosterone can both mitigate mortality risk while also safeguarding the heart from cardiovascular disease.
For  example, research released by the Journal of Clinical Endocrinology and Metabolism in June of 2012 provided the contradictory evidence of the JAMA study—and found that Testosterone Replacement significantly reduced mortality risk among veterans with Low-T by almost 40%. Those are findings that are hard to ignore.
example, research released by the Journal of Clinical Endocrinology and Metabolism in June of 2012 provided the contradictory evidence of the JAMA study—and found that Testosterone Replacement significantly reduced mortality risk among veterans with Low-T by almost 40%. Those are findings that are hard to ignore.
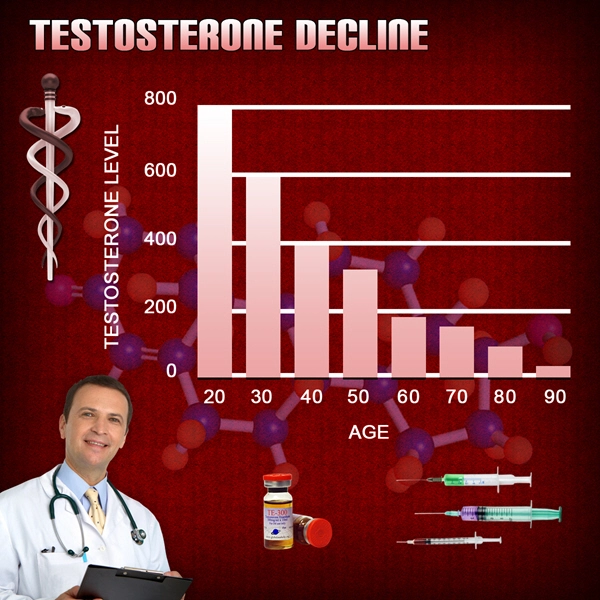
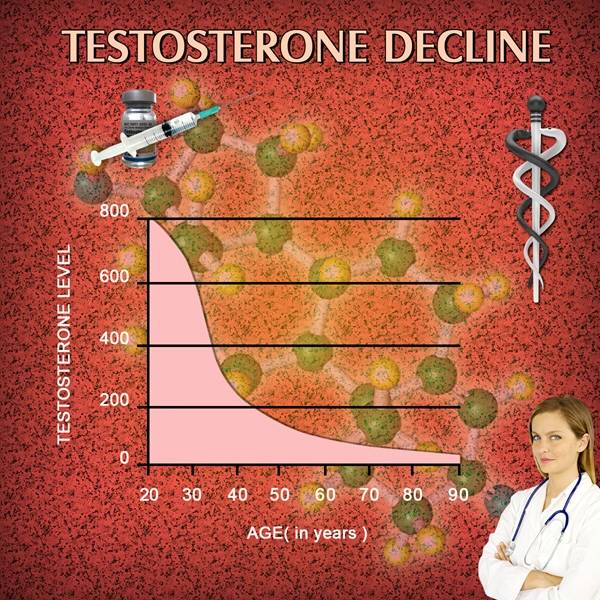
Testosterone Deficiency Leads to Increased Mortality Rates
It's also incredibly evident in the scientific literature that males with Clinical Testosterone Deficiency have significantly higher mortality rates than their peers.
Another study from JCEM, published in 2007, involving nearly 800 men from 50-91 years of age, presented evidence that men with deficient Testosterone Levels are at a much higher general mortality risk.
These patients were followed for a total of eleven years, and it was found that the bottom 25% of patients ranked by Serum Testosterone Concentrations had a 40 percent increased risk of death than those with normal Testosterone Levels. Low-T was also strongly correlated with cardiovascular disease.
How Can Testosterone Therapy Also Contribute to Heart Risk?
Now the JAMA study, when compared to the results of this 2007 JCEM study, begs the question—How can both Low Testosterone and Testosterone Therapy both be linked to increased mortality and heart disease risk? There are some reasons for this.
For example, in the JAMA study, the researchers explain that only six in ten patients ever had their Testosterone levels monitored after they were initially prescribed the therapy.
This is a significant issue because follow-up therapy is absolutely necessary both to assess the success of the treatment and to monitor for any potential side-effects. When undergoing testosterone therapy, one should get their testosterone levels measured via a blood test, every 3 months.
Insufficient Testosterone Dosage
It was also found that on average, the patients that received Testosterone Therapy did not receive enough of the treatment to provide optimal benefits associated with Low-T treatment.
Red Blood Cell Count Monitoring
Another major issue with this study is that two side-effects of Bio-Identical Testosterone Therapy were not adequately evaluated or mentioned—Red Blood  Cell count and Estradiol levels.
Cell count and Estradiol levels.
This is also a significant problem because many physicians that prescribe Testosterone to their patients don't pay enough attention to these two factors, which actually play the most prominent role in the more dangerous cardiovascular side-effects associated with Low-T therapy.
One of the easiest ways to lower one's red blood cell count is to get a blood test, the action of having one's blood drawn reduces the red blood cell count. Donating blood is also another option.
If these two factors are appropriately accounted for, the safety profile of Bio-Identical Testosterone increases dramatically.
Testosterone and Erythrocytosis
In many patients, Low-T replacement therapy leads to a condition known as Erythrocytosis, in which the bone marrow produces more Red Blood Cells than usual, potentially leading to issues such as hypertension and blood clotting which increase the risk of some severe cardiovascular maladies. This condition causes the blood to become too thick.
Dosage or Blood Testing/Donation
There are two simple ways to treat this condition and mitigate the risks associated with it—dropping the dosage or draining blood (which can be as simple as visiting the local Red Cross). Unfortunately, the patients analyzed in the JAMA research did not receive this care.
Testosterone and Estradiol
Furthermore, patients in the JAMA study were not adequately monitored for estradiol levels. As a part of the natural hormone cycle of the human body, some Testosterone is naturally turned into estradiol.
Elevated Estradiol
This is called aromatization. Elevated Estradiol levels are the mechanism by which the body tells the brain that Testosterone production is too high, which suppresses Testosterone Levels and brings Estrogen back into balance.
Of course, when you take Testosterone Therapy, the signals sent to the brain by Estrogen have no impact on Testosterone Concentrations, which elevates Estrogen levels.
Elevated Estrogen levels have long been associated with adverse cardiovascular issues in men. In the JAMA Testosterone Study, patients were not evaluated for Estrogen levels at any point, so there is no way to separate cardiovascular risk  resulting from Estrogen or Testosterone.
resulting from Estrogen or Testosterone.
Resolving the issues associated with elevated Estrogen levels is as easy as providing the patient with a single daily pill.
Arimidex (anastrozole) is an Estrogen blocker that suppresses the activity of Estrogen, including the negative effects associated with male cardiovascular profile.
The male body requires a specific level of Estrogen—not too high, and not too low. With the use of Estrogen Inhibitors and blood monitoring, it is possible to keep Estrogen Levels balanced, and it is possible to vastly improve the safety profile of Testosterone, which is not acknowledged in the JAMA literature.
High Testosterone and DHT
Another issue with Testosterone is when levels are too high, too much of the hormone gets converted into DHT, also known as Dihydrotestosterone.
The levels of DHT in the bloodstream are directly correlated with the levels of Testosterone, so if a patient receives too much Testosterone and does not get adequately evaluated, he puts himself at risks associated with elevated DHT Levels, including male pattern baldness, prostate enlargement, and cardiovascular disease.
Testosterone Therapy Safe if You Follow The Guidelines
As you can see, there are risks associated with Testosterone Therapy when monitoring is not conducted properly, but most of these risks are related to byproducts of Testosterone that are the result of overdose or underdosing, which can be easily prevented or mitigated with regular monitoring and adjustments in the testosterone protocol.
By choosing a knowledgeable Hormone Therapy Provider, you can get the most out of treatment while also minimizing the risks associated with such therapy.
 Don't let the risks outlined in this study prevent you from getting the care you need and deserve.
Don't let the risks outlined in this study prevent you from getting the care you need and deserve.
There is no reason to resign yourself to the slow physiological decline associated with Low-T. Talk to a licensed and board-certified clinical specialist to find out more.
Contact us to get your testosterone levels checked. We can speak with you about your options concerning testosterone deficiency and testosterone replacement therapy (TRT).
Reference
An update on heart disease risk associated with testosterone boosting
medications.
Contact Us Today For A Free Consultation

- Part 2: Effect of Testosterone Replacement Therapy on Prostate Tissue in Men with Late-Onset Hypogonadism (Dramatic Health) [Last Updated On: March 24th, 2018] [Originally Added On: May 7th, 2011]
- Full: Effect of Testosterone Replacement Therapy on Prostate Tissue in Men with Late-Onset Hypogonadism (Dramatic Health) [Last Updated On: May 3rd, 2023] [Originally Added On: May 7th, 2011]
- Testosterone Replacement Therapy (TRT): Optimizing Clinical Outcomes - Michael Aziz, MD [Last Updated On: November 12th, 2023] [Originally Added On: May 8th, 2011]
- Part 1: Effect of Testosterone Replacement Therapy on Prostate Tissue in Men with Late-Onset Hypogonadism (Dramatic Health) [Last Updated On: March 24th, 2018] [Originally Added On: May 8th, 2011]
- Part 4: Effect of Testosterone Replacement Therapy on Prostate Tissue in Men with Late-Onset Hypogonadism (Dramatic Health) [Last Updated On: November 12th, 2023] [Originally Added On: May 30th, 2011]
- Part 3: Effect of Testosterone Replacement Therapy on Prostate Tissue in Men with Late-Onset Hypogonadism (Dramatic Health) [Last Updated On: November 15th, 2023] [Originally Added On: June 2nd, 2011]
- Testosterone Replacement [Last Updated On: November 23rd, 2023] [Originally Added On: June 7th, 2011]
- Medical Professor on Testosterone Replacement Therapy [Last Updated On: November 17th, 2023] [Originally Added On: June 14th, 2011]
- Sean McCorkle Discusses Testosterone Replacement Therapy [Last Updated On: November 18th, 2023] [Originally Added On: July 11th, 2011]
- Use of Testosterone in Men With Prostate Cancer [Last Updated On: November 22nd, 2023] [Originally Added On: September 28th, 2011]
- Low Testosterone (Low T) - Video [Last Updated On: November 25th, 2024] [Originally Added On: December 10th, 2011]
- Transdermal Drug Delivery - Technologies, Markets, and Companies [Last Updated On: April 29th, 2025] [Originally Added On: February 2nd, 2012]
- How Testosterone Replacement Therapy Builds Muscle and Stops Pain [Last Updated On: February 4th, 2024] [Originally Added On: February 4th, 2012]
- Teva, BioSante’s Testosterone Gel for Men Wins Approval From U.S. FDA [Last Updated On: January 11th, 2018] [Originally Added On: February 15th, 2012]
- FDA approves Teva, BioSante testosterone gel [Last Updated On: January 18th, 2018] [Originally Added On: February 15th, 2012]
- Teva Fourth-Quarter Profit Rises on Cephalon Purchase [Last Updated On: January 16th, 2018] [Originally Added On: February 15th, 2012]
- Renowned Dr. Oz and the Acclaimed Financial Times Now Have Featured Dr. Lionel Bisson, Founder of ... [Last Updated On: April 27th, 2025] [Originally Added On: February 17th, 2012]
- Omaha man says testosterone replacement therapy changed his life [Last Updated On: December 15th, 2017] [Originally Added On: May 5th, 2012]
- Auxilium Pharmaceuticals, Inc. and GlaxoSmithKline LLC Enter Into a Co-Promotion Agreement for Testim® in the U.S. [Last Updated On: May 6th, 2025] [Originally Added On: May 21st, 2012]
- Hormone therapy results in weight loss [Last Updated On: January 27th, 2018] [Originally Added On: June 25th, 2012]
- Testosterone in Women-Putting Your Sex Drive Bacl On Track - Video [Last Updated On: December 31st, 2024] [Originally Added On: November 2nd, 2012]
- Men's Health PITCH: Testosterone - Video [Last Updated On: January 1st, 2025] [Originally Added On: November 2nd, 2012]
- Dr. Karron Power Appears on Nightline - Testosterone Therapy - Video [Last Updated On: January 1st, 2025] [Originally Added On: November 2nd, 2012]
- Testosterone Replacement Therapy: Who is TRT Best For? - Video [Last Updated On: January 2nd, 2025] [Originally Added On: November 2nd, 2012]
- Female sex-enhancing nasal spray undergoing clinical trials [Last Updated On: October 24th, 2015] [Originally Added On: November 2nd, 2012]
- Andropause: A Diagnosis Whose Time Has Come [Last Updated On: June 3rd, 2025] [Originally Added On: November 16th, 2012]
- Dealing With Mood Disorders During the Holidays (Depression, Anxiety, Depersonalization) - Video [Last Updated On: February 7th, 2025] [Originally Added On: November 26th, 2012]
- Testosterone Roundtable -- Hypergonadism and Testosterone Replacement Therapy (Part 6) - Video [Last Updated On: February 19th, 2025] [Originally Added On: December 10th, 2012]
- Battling my Testosterone Replacement Therapy Doctor, Carpal Tunnel Syndrome, and Weightlifting - Video [Last Updated On: March 12th, 2013] [Originally Added On: March 12th, 2013]
- Low T? Testosterone Replacement Therapy - Video [Last Updated On: March 13th, 2013] [Originally Added On: March 13th, 2013]
- Testosterone Replacement Therapy: Nothing To Be Ashamed Of: Strike First Nutrition - Video [Last Updated On: May 18th, 2013] [Originally Added On: May 18th, 2013]
- Testosterone Replacement Therapy: Symptoms of Low Testosterone - Strike First Nutrition - Video [Last Updated On: May 18th, 2013] [Originally Added On: May 18th, 2013]
- Testosterone Replacement Therapy Testimonial - Video [Last Updated On: June 15th, 2013] [Originally Added On: June 15th, 2013]
- Taurus Male Clinic Testosterone Replacement Therapy - Video [Last Updated On: July 28th, 2013] [Originally Added On: July 28th, 2013]
- Can I Quit TRT Or Testosterone Replacement Therapy? By Low Testosterone Expert Dr David Asher - Video [Last Updated On: March 16th, 2017] [Originally Added On: August 7th, 2013]
- What Are The Side Effects of TRT Testosterone Replacement Therapy? By Low T Expert Dr. David Asher - Video [Last Updated On: August 7th, 2013] [Originally Added On: August 7th, 2013]
- Bill Jones 1513 Testosterone Replacement Therapy Testimonial - Video [Last Updated On: August 8th, 2013] [Originally Added On: August 8th, 2013]
- 2013-08-06 Testosterone Replacement Therapy - Video [Last Updated On: August 10th, 2013] [Originally Added On: August 10th, 2013]
- Testosterone Replacement Therapy West Palm Beach Florida - Video [Last Updated On: August 18th, 2013] [Originally Added On: August 18th, 2013]
- Testosterone Replacement Therapy Testimony from Patient of Body Renew Medical in Lees Summit MO - Video [Last Updated On: September 2nd, 2013] [Originally Added On: September 2nd, 2013]
- FGSW - An Update On My Testosterone Replacement Therapy: Doctor's Visit 09.16.13 - Video [Last Updated On: September 19th, 2013] [Originally Added On: September 19th, 2013]
- Testosterone Replacement Therapy - Testosterone Treatment [Last Updated On: March 25th, 2025] [Originally Added On: October 31st, 2013]
- Testosterone Side Effects from Testosterone Replacement Therapy [Last Updated On: January 11th, 2018] [Originally Added On: November 3rd, 2013]
- FGSW - An Update On My Testosterone Replacement Therapy (TRT) 11.08.13: Getting No Sleep! - Video [Last Updated On: November 14th, 2013] [Originally Added On: November 14th, 2013]
- WebMD: Erectile Dysfunction: Testosterone Replacement Therapy [Last Updated On: December 6th, 2017] [Originally Added On: November 25th, 2013]
- Testosterone Replacement Therapy! Male Hormones! [Last Updated On: January 15th, 2018] [Originally Added On: November 25th, 2013]
- FGSW - Testosterone Replacement Therapy TRT Update: Am I Back Where I Started - 11.25.13 - Video [Last Updated On: November 27th, 2013] [Originally Added On: November 27th, 2013]
- The benefits and risks of testosterone replacement therapy: a ... [Last Updated On: January 12th, 2018] [Originally Added On: December 8th, 2013]
- Testosterone replacement therapy can carry health risks - CBS News [Last Updated On: January 16th, 2018] [Originally Added On: December 8th, 2013]
- Reclaim Your Energy and Sex Drive | Testosterone Replacement ... [Last Updated On: April 6th, 2025] [Originally Added On: December 21st, 2013]
- Low Testosterone Therapy and Treatment - Do You Have Low ... [Last Updated On: October 24th, 2015] [Originally Added On: December 24th, 2013]
- How Long Does it Take for Testosterone Replacement Therapy to ... [Last Updated On: December 30th, 2017] [Originally Added On: January 3rd, 2014]
- Testosterone Therapy - Bioidentical Testosterone Replacement [Last Updated On: January 23rd, 2018] [Originally Added On: January 9th, 2014]
- Transdermal testosterone replacement therapy - Video abstract 43475 - Video [Last Updated On: January 11th, 2014] [Originally Added On: January 11th, 2014]
- Testosterone Therapy - Bioidentical Testosterone Replacement ... [Last Updated On: December 21st, 2017] [Originally Added On: January 13th, 2014]
- Testosterone Side Effects from Testosterone Replacement ... [Last Updated On: December 8th, 2017] [Originally Added On: January 20th, 2014]
- MyAntiAgingMD The Leader In Testosterone Replacement Therapy - Video [Last Updated On: October 21st, 2020] [Originally Added On: January 29th, 2014]
- The benefits and risks of testosterone replacement therapy ... [Last Updated On: October 15th, 2020] [Originally Added On: February 6th, 2014]
- The Secret Female Hormone: How Testosterone Replacement Can Change Your Life [Last Updated On: October 28th, 2020] [Originally Added On: February 11th, 2014]
- Testosterone Replacement Therapy found to be linked to Heart Problems [Last Updated On: April 19th, 2025] [Originally Added On: February 25th, 2014]
- Serious Side Effects Linked to Testosterone Therapy [Last Updated On: September 17th, 2025] [Originally Added On: February 27th, 2014]
- Doctor Reveals How Getting off Testosterone Will Hurt Fighters on It [Last Updated On: November 27th, 2020] [Originally Added On: March 4th, 2014]
- California joins Nevada in banning testosterone replacement therapy [Last Updated On: October 4th, 2020] [Originally Added On: March 6th, 2014]
- Testosterone Replacement Therapy: How to Administer Expert TRT By John K. Crisler, DO - Video [Last Updated On: October 31st, 2020] [Originally Added On: March 9th, 2014]
- FGSW - Week 14 Weigh-In & Update: Going Back To The Endocrinologist - Video [Last Updated On: March 29th, 2014] [Originally Added On: March 29th, 2014]
- Drug Recall Attorney at Herrera Law Firm, Inc., Comments on Reported Link Between Testosterone Drugs and Heart Attack ... [Last Updated On: November 30th, 2020] [Originally Added On: April 2nd, 2014]
- FGSW - Testosterone Replacement Therapy Update 03.27.14: An Improvement?? - Video [Last Updated On: October 8th, 2020] [Originally Added On: April 2nd, 2014]
- FGSW Weekly Weigh In & Update 15 Still Working On Mobility 03 31 14 - Video [Last Updated On: October 15th, 2020] [Originally Added On: April 5th, 2014]
- Discover the risk of prostate cancer with testosterone replacement therapy - Video [Last Updated On: October 1st, 2020] [Originally Added On: April 5th, 2014]
- FGSW - Weekly Weigh In & Update 15: Still Working On Mobility 03.31.14 - Video [Last Updated On: October 3rd, 2020] [Originally Added On: April 7th, 2014]
- Testosterone Replacement Therapy - Video [Last Updated On: October 1st, 2020] [Originally Added On: April 12th, 2014]
- Reclaim Your Energy and Sex Drive | Testosterone ... [Last Updated On: April 21st, 2025] [Originally Added On: April 14th, 2014]
- Low Testosterone Claims: Options in a Growing Class Action Suit - Video [Last Updated On: November 25th, 2020] [Originally Added On: April 26th, 2014]
- Acrux falls 15% on sales warning [Last Updated On: September 28th, 2025] [Originally Added On: April 28th, 2014]
- Testosterone Replacement Therapy in Men - myVMC [Last Updated On: November 1st, 2020] [Originally Added On: April 30th, 2014]
- NJ-Based Law Firm Exploring Potential Legal Claims from Side Effects of Testosterone Replacement Therapy [Last Updated On: October 22nd, 2020] [Originally Added On: May 1st, 2014]
- Viewer Mail - Testosterone Replacement Therapy/TRT Not Natty, Balls Busted, etc. - Video [Last Updated On: October 2nd, 2020] [Originally Added On: May 4th, 2014]
- Seen At 11: Experts Urge Caution When Using Popular Hormone Replacement Therapy [Last Updated On: November 11th, 2020] [Originally Added On: May 10th, 2014]
- Are Low-T Drugs Putting Patients At High Risk? [Last Updated On: October 15th, 2020] [Originally Added On: May 10th, 2014]
- Seen At 11: Testosterone Replacement Therapy Could Come With Serious Side Effects - Video [Last Updated On: May 11th, 2014] [Originally Added On: May 11th, 2014]
Word Count: 1308