Introduction
Hypopituitarism, a condition characterized by the reduced secretion of one or more of the hormones produced by the pituitary gland, has been increasingly recognized as a significant factor in the development of osteoporosis among American males. Osteoporosis, traditionally viewed as a condition primarily affecting postmenopausal women, is now understood to pose a substantial risk to men, particularly those with hypopituitarism. This article delves into the prospective study conducted to elucidate the role of hypopituitarism in the development of osteoporosis and its implications for bone health in American males.
The Pathophysiology of Hypopituitarism and Osteoporosis
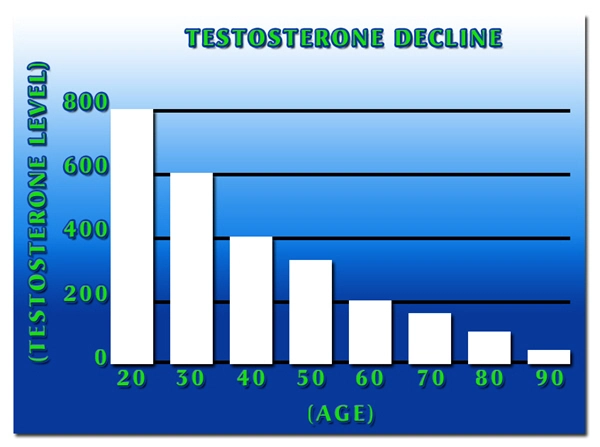
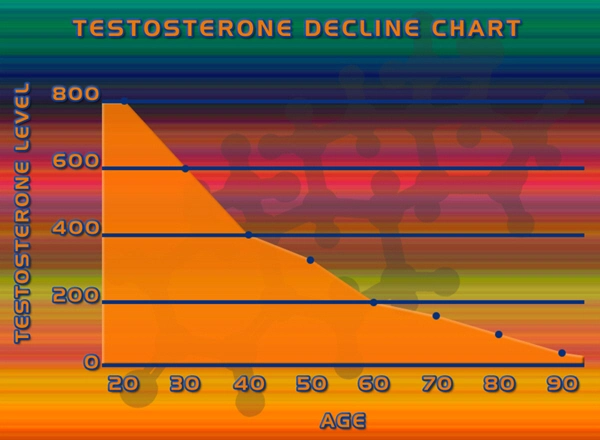
Hypopituitarism can lead to deficiencies in hormones such as growth hormone (GH), thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), and gonadotropins (LH and FSH). These hormonal deficiencies can disrupt the normal metabolic processes that maintain bone density and strength. Specifically, GH deficiency is known to impair bone formation, while deficiencies in gonadotropins can lead to reduced testosterone levels, which are crucial for maintaining bone mass in men. The study found that American males with hypopituitarism exhibited significantly lower bone mineral density (BMD) compared to their healthy counterparts, highlighting the direct impact of hormonal imbalances on bone health.
Study Design and Methodology
The prospective study involved a cohort of 200 American males diagnosed with hypopituitarism, aged between 30 and 70 years. Participants were followed over a five-year period, during which their BMD was assessed annually using dual-energy X-ray absorptiometry (DXA). Additionally, serum levels of relevant hormones were measured at baseline and annually to monitor hormonal status and its correlation with BMD changes. The control group consisted of 200 age-matched healthy males without hypopituitarism.
Findings and Clinical Implications
The study revealed a significant decline in BMD among the hypopituitarism group, with an average annual decrease of 1.5% in the lumbar spine and 1.2% in the femoral neck. In contrast, the control group showed a much slower rate of BMD decline, averaging 0.3% annually. These findings underscore the accelerated bone loss associated with hypopituitarism. Furthermore, the study identified a strong correlation between the severity of hormonal deficiencies and the extent of BMD reduction, suggesting that early and aggressive hormonal replacement therapy could be crucial in mitigating the risk of osteoporosis in affected individuals.
Management and Treatment Strategies
Effective management of hypopituitarism in American males requires a multifaceted approach. Hormone replacement therapy (HRT) tailored to the specific deficiencies identified in each patient is essential. For instance, GH replacement has been shown to improve BMD in patients with GH deficiency. Similarly, testosterone replacement therapy can help restore bone mass in those with hypogonadism. The study advocates for regular monitoring of BMD and hormonal levels to adjust treatment regimens as needed, ensuring optimal bone health outcomes.
Public Health and Awareness
Raising awareness about the link between hypopituitarism and osteoporosis is vital for improving health outcomes among American males. Public health initiatives should focus on educating both healthcare providers and the general public about the importance of early diagnosis and treatment of hypopituitarism. Encouraging men to undergo regular health screenings, particularly those with a family history of pituitary disorders or osteoporosis, can facilitate early intervention and prevent the progression to severe bone loss.
Conclusion
The prospective study on the role of hypopituitarism in the development of osteoporosis in American males provides compelling evidence of the significant impact of hormonal deficiencies on bone health. By understanding the pathophysiology and implementing targeted treatment strategies, healthcare providers can effectively manage this condition and improve the quality of life for affected individuals. Continued research and public health efforts are essential to further elucidate the mechanisms involved and enhance preventive and therapeutic approaches.
Contact Us Today For A Free Consultation

- What is Hypopituitarism [Last Updated On: March 16th, 2025] [Originally Added On: February 18th, 2021]
- Is There Such a Thing as Too Much HGH? [Last Updated On: March 16th, 2025] [Originally Added On: August 22nd, 2023]
- Unveiling the Cardiovascular Implications of Hypopituitarism in American Males [Last Updated On: March 1st, 2025] [Originally Added On: March 1st, 2025]
- Hypopituitarism in American Men: Impacts and Management Strategies [Last Updated On: March 10th, 2025] [Originally Added On: March 10th, 2025]
- Hypopituitarism and Metabolic Syndrome: Unraveling the Connection in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Unveiling the Cardiovascular Risks: The Link Between Hypopituitarism and Heart Disease in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Unraveling the Connection: Hypopituitarism and Uterine Fibroids in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Exploring Hypopituitarism's Impact on Vaginal Health and the Female Reproductive System [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Unraveling the Hormonal Link: Hypopituitarism and Breast Cancer in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Hypopituitarism and Autoimmune Disorders: Critical Insights for American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Hypopituitarism and Obesity in American Males: Hormonal Impacts and Management Strategies [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Hypopituitarism in American Males: Hormonal Imbalances and Sleep Disorder Connections [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Surgical Interventions for Hypopituitarism and Pituitary Tumors in American Males [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Hypopituitarism's Impact on Mental Health in American Males: Depression, Anxiety, and Treatment [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Multidisciplinary Care Essential for Managing Hypopituitarism in American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Hypopituitarism in American Males: Cancer Risks and Monitoring Strategies [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Hypopituitarism and Anemia in American Males: The Critical Role of EPO Deficiency [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Hypopituitarism and Male Hair Loss: Hormonal Mechanisms and Treatment Strategies [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Hypopituitarism's Impact on Kidney Function in American Males: Monitoring and Management [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Hypopituitarism's Impact on Immune Function in American Men: Diagnosis, Treatment, and Management [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Hypopituitarism in American Males: Cognitive Impacts and Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hypopituitarism in American Males: Impact on Eye Health and Visual Impairments [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hypopituitarism in Aging American Males: Impact, Diagnosis, and Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hypopituitarism's Impact on Liver Health in American Males: Hormonal Deficiencies and Management [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hypopituitarism's Impact on Joint Health in American Males: Diagnosis and Management [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hypopituitarism's Impact on GI Health in American Males: Digestion and Nutrient Absorption [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypopituitarism's Impact on Skin Health in American Males: Symptoms and Management [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypopituitarism and Seizure Disorders in American Males: Clinical Insights and Management [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypopituitarism and Migraines: Hormonal Links and Management Strategies for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypopituitarism and Hypertension: Impact on Blood Pressure in American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypopituitarism's Link to Gout and Uric Acid in American Males: A Comprehensive Analysis [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypopituitarism's Impact on Muscle Strength in American Males: Management and Insights [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Autoimmune Link: Hypopituitarism and Rheumatoid Arthritis in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Exploring the Link Between Hypopituitarism and MS in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Autoimmune Link Between Hypopituitarism and Celiac Disease in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Hypopituitarism and Diabetes: Impact on Glucose Metabolism in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypopituitarism's Impact on Kidney Health in American Males: Monitoring and Management [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypopituitarism and Hearing Loss: Exploring Links and Implications for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypopituitarism in American Males: Cardiovascular Risks and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypopituitarism's Impact on Asthma in American Males: Hormonal Insights and Management [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypopituitarism and Allergies: Hormonal Impacts on Immune Response in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism's Role in Accelerating Parkinson's Disease in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism and Liver Cirrhosis: Impacts and Management in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism and CFS Overlap in American Males: Symptoms, Mechanisms, and Clinical Insights [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism and Fibromyalgia: Overlapping Symptoms and Impact on American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism, Hormonal Imbalances, and Alzheimer's Risk in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism and Sjögren's Syndrome: Effects on Exocrine Glands in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism and Dyslipidemia: Impacts on American Males' Health and Management Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypopituitarism's Impact on Prostate Cancer in American Males: Diagnosis and Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Exploring the Link Between Hypopituitarism and Lupus in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypopituitarism and Pituitary Cancer: Early Detection and Management for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypopituitarism in American Males: Monitoring Hormones to Reduce Stroke Risk [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypopituitarism and IBD: Gastrointestinal Links and Impacts on American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypopituitarism and Adrenal Cancer: Endocrine Links in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypopituitarism and Osteoarthritis: Impact on Joint Health in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Hypopituitarism and Gallbladder Disease: Exploring Links in American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Hypopituitarism's Impact on Pancreatitis: Risks and Management for American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Hypopituitarism and Breast Cancer Link in American Males: Hormonal Insights and Clinical Implications [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Hormonal Imbalances in Hypopituitarism and Thyroid Cancer: Impacts on American Males [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Hypopituitarism and Testicular Cancer: Impacts and Fertility Preservation Strategies [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Hypopituitarism and Ovarian Cancer: Exploring Hormonal Links in American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Hypopituitarism in American Males: Hormonal Imbalances and Benign Tumor Risks [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Hypopituitarism and PCOS: Symptoms, Diagnosis, and Management Strategies [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Hormonal Links Between Hypopituitarism and Endometriosis in American Males Explored [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Hypopituitarism and Erectile Dysfunction: Hormonal Links and Holistic Management in American Males [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Hypopituitarism: Effects on Male Reproductive and Penile Health [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Hypopituitarism, Hormonal Imbalance, and Cervical Cancer Risk in Men [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Hypopituitarism's Impact on Female Reproductive and Vaginal Health: Diagnosis and Management [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Hypopituitarism and Premature Ejaculation: Exploring Hormonal Links in American Males [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Hypopituitarism's Impact on Miscarriage Risk and Male Fertility in America [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Hypopituitarism and Preeclampsia in Pregnancy: Monitoring and Management Strategies [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Hypopituitarism and Ectopic Pregnancy: Impacts and Management in Women's Health [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Hypopituitarism and Male Infertility: Causes, Diagnosis, and Treatment Options [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Hypopituitarism and Gestational Diabetes: Metabolic Links in American Males [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Hypopituitarism's Impact on Lactation: Support Strategies for American Males [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Hypopituitarism's Impact on Mental Health and Postpartum Depression in American Males [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Hormonal Imbalances in Women: Hypopituitarism, Menopause, and Supportive Roles for American Males [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Hypopituitarism's Impact on Dental Health in American Males: Monitoring and Care Strategies [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Hypopituitarism and Andropause: Impacts and Management in Aging American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Hypopituitarism and Alopecia: Impact on Male Hair Health and Treatment Strategies [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
Word Count: 588