Introduction to Testosterone's Role in Bladder Health
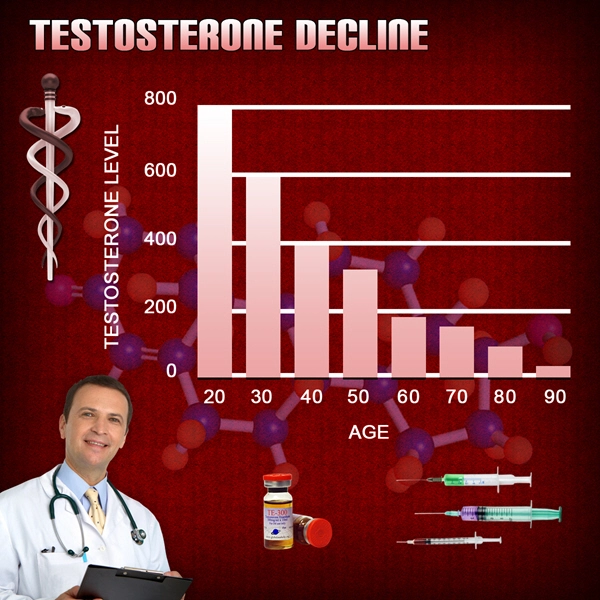
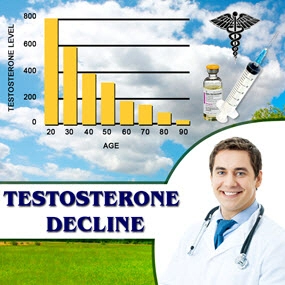
Testosterone, a key male sex hormone, not only plays a pivotal role in sexual and reproductive function but also impacts various other physiological systems, including the urinary system. Its influence extends to the structural and functional integrity of the bladder, particularly the smooth muscle tissue critical for normal bladder function. Chronic testosterone deficiency, a condition commonly observed in the aging male population, has been associated with various urinary symptoms. However, the ultrastructural changes in bladder smooth muscle cells (SMCs) under the condition of low testosterone levels have not been extensively studied.
Electron Microscopy and Bladder Smooth Muscle Analysis
Recent advances in electron microscopy have provided new insights into the cellular and subcellular structures of bladder SMCs affected by testosterone deficiency. This imaging technique, due to its high resolution, allows for the detailed observation of ultrastructural changes that could elucidate the pathophysiological mechanisms underlying bladder dysfunction in testosterone-deficient males.
Key Findings from Recent Studies
Research employing electron microscopy to analyze bladder SMCs in the context of testosterone deficiency has highlighted several critical changes. The studies generally show that testosterone-deficient states are associated with notable alterations in the morphology and function of bladder smooth muscle. These changes include:
1. **Degradation of Smooth Muscle Fibers**: There is a noticeable degradation and disorganization of smooth muscle fibers, which are essential for the contractility and structural integrity of the bladder. This degradation potentially leads to decreased bladder capacity and stability, contributing to clinical symptoms such as urinary incontinence and increased frequency.
2. **Mitochondrial Abnormalities**: Mitochondria, the energy powerhouses of the cell, show signs of dysfunction and structural alterations. This could affect the energy supply necessary for muscle contraction and repair processes, further impairing bladder function.
3. **Alterations in Extracellular Matrix (ECM)**: The ECM, which provides support and maintains the architectural structure of tissues, shows signs of remodeling and increased fibrosis. An altered ECM can lead to stiffness and reduced elasticity of the bladder wall, impacting its ability to expand and contract effectively.
4. **Changes in Cell Junctions**: The integrity of cell junctions, which are crucial for cell-to-cell communication and structural cohesion, is compromised. This disruption can affect the coordinated activity of SMCs during the bladder filling and voiding phases.
Implications for Clinical Management
These ultrastructural changes suggest that chronic testosterone deficiency could directly impair bladder function by altering the structural and functional properties of bladder SMCs. This understanding is crucial for developing targeted therapies that could mitigate these changes. Potential therapeutic approaches may include testosterone replacement therapy (TRT), which has been shown in some studies to reverse some of the adverse effects of testosterone deficiency on muscle tissue, including that of the bladder.
Conclusion and Future Directions
The insights provided by electron microscopy into the ultrastructural effects of chronic testosterone deficiency on bladder smooth muscle offer a deeper understanding of the pathophysiological basis for urinary symptoms in affected males. Future research should focus on longitudinal studies to track these changes over time and evaluate the efficacy of testosterone replacement and other therapeutic strategies in ameliorating these structural and functional alterations. Such studies are essential for improving the quality of life of those suffering from testosterone deficiency and associated bladder health issues.
Contact Us Today For A Free Consultation

- Unveiling the Role of Prostatic Acid Phosphatase in Monitoring Androgen Activity During Testosterone Replacement Therapy in Men [Last Updated On: February 21st, 2025] [Originally Added On: February 21st, 2025]
- Understanding Urethral Epithelial Atrophy: Impact, Diagnosis, and Hormone Replacement Therapy [Last Updated On: March 8th, 2025] [Originally Added On: March 8th, 2025]
- Testosterone's Impact on Prostatic Stroma: Implications for Prostate Health and Therapy [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Alpha1-Adrenoreceptor Density, Testosterone, and LUTS Severity in American Men: Clinical Insights [Last Updated On: March 11th, 2025] [Originally Added On: March 11th, 2025]
- Exploring the Impact of Hormone Replacement on Pelvic Floor Electromyographic Activity in Hypogonadal Men [Last Updated On: March 12th, 2025] [Originally Added On: March 12th, 2025]
- Exploring the Dynamics of Post-Void Residual Volume in Men with Testosterone Deficiency: A Longitudinal Study on Testosterone Replacement Therapy [Last Updated On: March 13th, 2025] [Originally Added On: March 13th, 2025]
- Androgen-Dependent Regulation of PDE5 in Prostatic Tissue: A New Frontier in Men's Urological Health [Last Updated On: March 14th, 2025] [Originally Added On: March 14th, 2025]
- Unveiling New Biomarkers: The Role of Urinary Proteomics in Diagnosing Lower Urinary Tract Dysfunction in Androgen-Deficient Men [Last Updated On: March 15th, 2025] [Originally Added On: March 15th, 2025]
- Urinary Flow Cytometry: A Non-Invasive Tool for Monitoring Hypogonadism and TRT Effects [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Vesicourethral Reflux in Hypogonadal Men: Hormonal and Bladder Neck Dysfunction Insights [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Ultrasonographic BWT and Urodynamic Parameters in American Men with Late-Onset Hypogonadism [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Prostatic Aromatase in Aging Men: Risks and Management in Testosterone Therapy [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Androgen-Regulated Genes in Urothelium: Impact of Hormone Therapy on Men's Health [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Mitochondrial Function in Bladder Smooth Muscle of Testosterone-Deficient Men: Insights and Implications [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Prostatic Inflammation in Hypogonadal Men: Histopathology and Testosterone Therapy Effects [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- TRT's Impact on Prostate Health: Insights from Color Doppler Ultrasonography [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Metabolomic Analysis of Prostatic Fluid in Testosterone-Deficient Men: Urological Implications and Treatment Responses [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Testosterone's Impact on Bladder ECM: GAGs, Proteoglycans, and Male Urological Health [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Urinary Exosomal microRNAs: Biomarkers for Hypogonadism and LUTS in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Testosterone Deficiency and Urinary Stone Risk: Crystallization Patterns in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Testosterone's Impact on Prostatic Gap Junction Proteins and TRT Implications for American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Testosterone Deficiency Impacts Autonomic Innervation and Male Urological Health [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Neural Density in Detrusor Muscle: Hypogonadism's Urological Impact and Management [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Prostatic Neuroendocrine Cells in Androgen-Deficient Men: Analysis and HRT Response [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Testosterone Therapy's Impact on PSA Kinetics and Safety Monitoring in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Testosterone Deficiency and Bladder Function: Insights from Ambulatory Urodynamic Monitoring [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Urethral Pressure Changes in Hypogonadal Men Before and After Androgen Therapy [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Androgen Deficiency Impacts Bladder Contractile Proteins in American Men: Proteomic Insights [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- TRT's Impact on Prostate Health: Assessing Stiffness with Transrectal SWE in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- TRT's Impact on Micturition Parameters and Serum Hormone Levels in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Prostatic Calcifications in Hypogonadal Men: Prevalence, Composition, and LUTS Association [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Androgen Receptor Distribution in Hypogonadal Men's Lower Urinary Tract: Clinical Insights [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Testosterone Normalization Effects on Bladder Pressure in Deficient Men: Cystometry Insights [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Testosterone Replacement Therapy Enhances Bladder Function in Deficient American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Videourodynamic Assessment and Hormone Therapy for Postvoid Dribbling in Testosterone-Deficient Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- TRT Enhances Uroflowmetric Parameters in American Men: A Comprehensive Study [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Prostatic Urothelial Metaplasia in Hypogonadal Men: Prevalence, Implications, and Testosterone Therapy [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Testosterone Therapy's Impact on Prostatic Growth Factors and Hyperplasia Risk [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Uroflowmetry and Hormonal Correlations in American Men with Androgen Deficiency [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Testosterone Deficiency and Detrusor Overactivity: Urodynamics and Hormone Therapy Effects [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Testosterone Therapy in Hypogonadal Men: PIN Incidence and Surveillance Protocols [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- TRT-Induced Ultrastructural Changes in Prostatic Smooth Muscle: An Electron Microscopy Study [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Non-Bacterial Prostatitis and Hypogonadism: Exploring Inflammation and Testosterone Therapy Benefits [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Bladder Neck Collagen in Hypogonadal Men: Urodynamic Impacts and Therapeutic Insights [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Doppler Ultrasonography Monitors Prostatic Flow Changes in American Men on TRT [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone Therapy's Impact on Prostatic Tissue in Hypogonadal Men: A Morphometric Study [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone Fluctuations and Maximum Flow Rate Variability in Hypogonadal Men on TRT [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone Deficiency and Nocturnal Polyuria: Mechanisms and Hormone Therapy in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- PSMA Expression Analysis in Androgen-Deficient Men Before and After Hormone Therapy [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone Therapy Enhances Urethral Sphincter Function in Hypogonadal Men: EMG Insights [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Testosterone Therapy's Impact on Prostate Health: A Histomorphometric Analysis [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Prostatic Stromal Androgen Receptors: Key to Managing LUTS in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Androgen Therapy Modulates Apoptotic Index in Hypogonadal Men's Prostatic Epithelium [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- LOH Impact on Bladder Compliance: Urodynamic and Hormonal Insights in Aging Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- DSD in Androgen-Deficient Men: Prevalence, Urodynamics, and Hormonal Insights [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Neurogenic Bladder in Hypogonadal Men with Metabolic Syndrome: Urodynamics and Hormonal Insights [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Androgen Deficiency's Impact on Detrusor Oxygen Tension and Testosterone Therapy Benefits [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Testosterone Deficiency Impacts Prostatic Secretions and Urological Health in American Males [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Bladder Sensation Mapping in Testosterone-Deficient Men: QST Before and After HRT [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- 3D Ultrasonography: Monitoring Prostate Health in Men on Testosterone Therapy [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Testosterone Deficiency Impacts Bladder Capacity: HRT Benefits in American Males [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Prostatic Aromatase Activity and Estrogen's Role in LUTS Among Aging American Men [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Computerized Urethral Pressure Analysis in Hypogonadal Men Pre- and Post-TRT [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Androgen Receptor Sensitivity: Predicting Testosterone Therapy Outcomes in Men's Urological Health [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Testosterone Deficiency and Bladder Health: Suburothelial Myofibroblast Insights for American Men [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Bladder Wall Fibrosis in Men: Grading, Testosterone Deficiency, and Hormone Therapy Benefits [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Prostatic Elastography: Assessing Tissue Stiffness in Men on Testosterone Therapy [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Diurnal LUTS Variations in Hypogonadal Men Linked to Testosterone Rhythms [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- TRT Modulates Prostatic Epithelial Cell Autophagy in Hypogonadal Men: A Review [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- OAB in Androgen-Deficient Men: Prevalence, Symptoms, and Testosterone Therapy Benefits [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- TRT Enhances Periurethral Vascularity in American Men: Power Doppler Insights [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Differentiating and Treating Prostatitis-like Symptoms in Hypogonadal Men with Testosterone Therapy [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Intraprostatic Hormone Levels in American Men: Testosterone Therapy Impacts and Management [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Mathematical Modeling Predicts Prostatic Growth in TRT for American Men [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Electrophysiological Insights into Bladder Nerve Activity in Testosterone-Deficient American Males [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Neurourological Assessment Protocol for Autonomic Neuropathy in Testosterone-Deficient American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Testosterone Deficiency and Urinary GAG Levels: Biochemical Insights and Clinical Implications [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Testosterone Therapy Enhances VUJ Functionality in Androgen-Deficient Men: Videourodynamic Insights [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Urinary NGF as Biomarker for LUTS in Testosterone-Deficient Men: Diagnostic Potential [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- CEUS: A Novel Approach to Assess Urethral Mucosal Vasocongestion in Hypogonadal Men [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
Word Count: 529