Hypogonadism is a condition where the sex glands produce little or no sex hormones. The sex glands are the testes in men and the ovaries in women. Testosterone is produced in the testes and estrogen is produced in the ovaries. These are the two main sex hormones produced by men and women, respectively.
Hypogonadism is a condition where the sex glands produce little or no sex hormones. The sex glands are the testes in men and the ovaries in women. Testosterone is produced in the testes and estrogen is produced in the ovaries. These are the two main sex hormones produced by men and women, respectively.
Sex hormones control sexual characteristics, such as breast and testicular development as well as pubic hair growth. In addition, both testosterone and estrogen play major roles in the male and female reproductive systems, including menstrual cycles and sperm production. Humans would not survive without sex hormones!
Video Link: https://vimeo.com/415714562
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
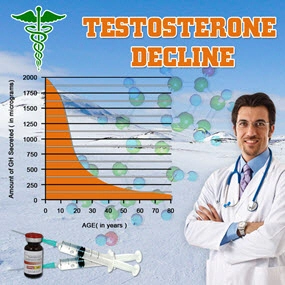
Hypogonadism is also called gonad deficiency. In males, it may be called low testosterone/andropause and in women, prior to menopause, primary ovarian insufficiency. Thankfully, hypogonadism can usually be easily treated with hormone replacement therapy (HRT).
Types of Hypogonadism
There are two types: primary and central. Primary hypogonadism occurs when the gonads, or sex organs, have an issue in sex hormone production. The cells in the gonads are receiving the hormonal messages from the brain to produce testosterone or estrogen, but for some reason aren't doing so.
Central, or secondary, hypogonadism occurs when the hypothalamus and pituitary gland in the brain are not sending the right signals and one or both of them are experiencing issues doing their jobs. They are supposed to produce the hormone messengers that travel to the gonads and signal them to produce the sex hormones.
So What Causes Hypogonadism?
In primary hypogonadism, the causes include:
- autoimmune disorders: a condition where your immune system is accidentally attacking itself instead of foreign infectious agents. The immune system will mistake different cells of your body as a foreign agent such as protective coverings of nerves (multiple sclerosis), the joints (rheumatoid arthritis) or even the entire body (Lupus).
- Turner syndrome: a genetic condition that only affects females where one of her X chromosomes is missing or just partially missing. It requires ongoing medical care and causes several developmental issues including heart defects, failure of ovaries to develop and short height.
- Klinefelter syndrome (XXY Syndrome): a genetic condition that only affects males where he is born with an extra X chromosome copy. Symptoms and signs include smaller than normal testicles, reduced muscle mass, body and facial hair and enlarged breast tissue. It can lead to reproductive issues due to decreased sperm production.
- undescended testes (cryptorchidism): This happens before a baby is born and is when a testicle does not move down into the scrotum. It does require treatment as there is a higher risk of testicular cancer, torsion and the development of a hernia near the groin. Normally, the testicles descend into the scrotum because sperm cannot be produced at body temperature. If both testicles are affected, this can lead to infertility.
- radiation exposure: Exposure sources include chemotherapy and especially scatter radiation when patients with rectal cancer are treated with pelvic radiation. Other cancers can be treated with radiation therapy as well, leading to exposure. The radiation can damage the testicles, leading to impaired testosterone production.
- liver and kidney diseases: Chronic alcoholism, causing liver disease or impairment, leads to an impaired hypothalamic-pituitary axis. Systemic diseases can indirectly harm testicular function via gonadotropin suppression and eventually cause testicular failure. Testicular failure is associated with liver disease, alcoholism, chronic renal disease, rheumatic diseases and others.
- mumps involving the testicles: Mumps is caused by a virus and causes the swelling of the salivary glands and jaw. If the disease makes its way to the testicles, it can damage them. This damage can then affect testosterone production.
In central hypogonadism, the causes include:
- Kallmann syndrome (atypical development of the hypthalamus): The production of hormones in the hypothalamus that affect sexual development is impaired. Boys suffer from micropenis and undescended testicles. Secondary sex characteristics will also not develop during puberty. The hypothalamus is not producing enough testosterone.
- obesity: The most significant risk factor for testosterone deficiency in men. Obesity can cause increased levels of several hormones including oestrogens and causes hormonal imbalance. Hypogonadism itself can cause more weight gain, thus creating a self-perpetuating cycle.
- nutritional deficiencies: If the body is not getting proper nutrition, this can negatively affect the hypothalamic-gonadotropin hormonal axis. This is especially seen in girls who have eating disorders, causing amenorrhea (temporary loss of menstruation). The hormones insulin and leptin, which are affected by food intake and nutrition, are important links between nutrition and the gonadotropin axis. The adverse effects can be reversed.
- inflammatory diseases: These diseases include allergies, inflammatory bowel disease, autoimmune, hepatitis, etc. Chronic inflammation can cause damage to the body's healthy tissues and if these tissues include the gonads, hypogonadism can result.
- HIV: It is common to see HIV patients also exhibiting low testosterone levels -- approximately 70% of patients.
- pituitary gland or hypothalamic injury: An injury to the pituitary gland or hypothalamus, either physical trauma from an accident or from radiation can cause disproportionate hormonal release and signaling.
- pituitary gland tumors: These are also called pituitary adenomas and are noncancerous tumors that do not spread past the skull. A tumor can cause the pituitary gland to release either too many or too little of the hormones it typically releases. Symptoms include hormonal imbalance, headaches and loss of vision from pressure.
- opioid or steroid use/abuse: This is also called opioid-induced endocrinopathy when the opioid use suppresses the sex hormones. In general, opioids lower the levels of oxytocin, testosterone and estradiol in the human body.
Symptoms of Hypogonadism
Women who have primary ovarian insufficiency may experience:
- slow or no breast growth
- body hair loss
- low or no sex drive
- hot flashes
- lack of menstruation
- breast discharge
Men who have low testosterone may experience:
- body hair loss
- breast growth
- reduced growth of penis and testicles
- muscle loss
- hot flashes
- low or no sex drive
- erectile dysfunction
- fatigue
- infertility
Diagnosis of Hypogonadism
 The first step in diagnosing hypogonadism is a physical exam. An examination of the amount of body hair, muscle mass and sex organ growth is compared to the standard amount or growth expected for the age range of the patient.
The first step in diagnosing hypogonadism is a physical exam. An examination of the amount of body hair, muscle mass and sex organ growth is compared to the standard amount or growth expected for the age range of the patient.
The next step involves a blood test. The level of sex hormones is measured as well as follicle-stimulating hormone (FSH) and luteinizing hormone. Both of these hormones work together in the male and female body to regulate the developments, growth and maturation of the reproductive system.
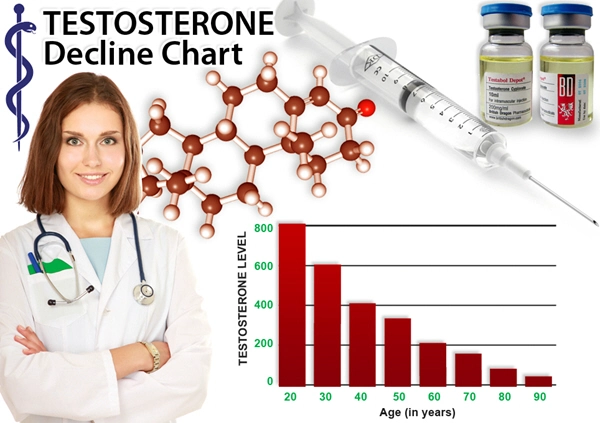
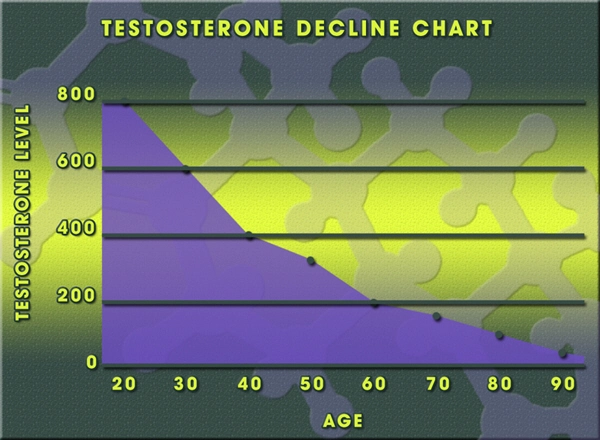
Both estrogen and testosterone levels are highest in the morning and this is when the blood will be drawn. Men may also be asked to supply a semen sample to check the sperm count as hypogonadism can lower a man's sperm count.
 Other measurements may be taken including iron, prolactin and thyroid hormones. Hypogonadism symptoms are sometimes mistaken for thyroid issues as they both involve hormonal imbalance. Iron has a tendency to affect the levels of sex hormones in your blood. Prolactin is another hormone that promotes breast development and the production of breast milk. It's a good idea to check the levels of several hormones if hypogonadism is suspected to get more of a bigger picture as to what exactly is going on and what is high/low.
Other measurements may be taken including iron, prolactin and thyroid hormones. Hypogonadism symptoms are sometimes mistaken for thyroid issues as they both involve hormonal imbalance. Iron has a tendency to affect the levels of sex hormones in your blood. Prolactin is another hormone that promotes breast development and the production of breast milk. It's a good idea to check the levels of several hormones if hypogonadism is suspected to get more of a bigger picture as to what exactly is going on and what is high/low.
Lastly, an ultrasound may be used to look at the ovaries to check for cysts or polycystic ovary syndrome. MRIs or CT scans could be ordered to check for tumors on the pituitary gland.
Treatment of Hypogonadism
For women, the best treatment will be increasing the amount of sex hormones, such as estrogen therapy. This could be via patches or pills. If the female patient experiences low sex drive, she may be prescribed low doses of testosterone.
For men, testosterone replacement therapy will be utilized. The methods of supplementing testosterone include injections, patches, gels or creams.
 Hypogonadism is a chronic condition and will most likely need to be treated for life, depending on what caused it. If it was caused by nutritional deficiencies, it may be easily corrected by supplementing with the lacking nutrients. If it is from a tumor on the pituitary gland, removal of the tumor may get things back in working order. Otherwise, once treatment is stopped, the sex hormone levels may decrease again.
Hypogonadism is a chronic condition and will most likely need to be treated for life, depending on what caused it. If it was caused by nutritional deficiencies, it may be easily corrected by supplementing with the lacking nutrients. If it is from a tumor on the pituitary gland, removal of the tumor may get things back in working order. Otherwise, once treatment is stopped, the sex hormone levels may decrease again.
If you think you may be suffering from hypogonadism (low testosterone or primary ovarian insufficiency) feel free to contact our HRT clinic to discuss your symptoms and how to get tested for the condition. We have representatives available to talk for free with no-obligation about any concerns you may have. Contact us via the contact form or simply give us a call!
Contact Us Today For A Free Consultation

- BioSante Pharmaceuticals, Inc. to Present at BIO Investor Forum [Last Updated On: March 16th, 2025] [Originally Added On: October 9th, 2012]
- Secondary osteoporosis: More than what meets the eye! [Last Updated On: March 16th, 2025] [Originally Added On: October 10th, 2012]
- Trimel Provides Clinical and Operational Update [Last Updated On: March 16th, 2025] [Originally Added On: October 15th, 2012]
- Obese teen boys likelier to become impotent and infertile adults [Last Updated On: March 16th, 2025] [Originally Added On: October 17th, 2012]
- Obese teen boys have up to 50 percent less testosterone than lean boys [Last Updated On: March 16th, 2025] [Originally Added On: October 17th, 2012]
- Trimel Reports Physician Market Research Results for CompleoTRT(TM) [Last Updated On: March 16th, 2025] [Originally Added On: October 24th, 2012]
- Obese teen boys likelier to turn into 'impotent' men [Last Updated On: March 16th, 2025] [Originally Added On: October 24th, 2012]
- Trimel Pharmaceuticals Corporation to Report Third Quarter 2012 Results and Host a Conference Call to Update Investors [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Peer Exchange: Establishing Bone Health Clinics - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- What is hypogonadism and how does it affect fertility? - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Low Testosterone in Men or Man-O-Pause - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Propecia (Finasteride) -- Undisclosed Mechanisms, Potential Dangers [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- How to Get Ripped - Why You Shouldnt Use Anabolic Steroids - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Future Doc: Andropause Alternatives with Dr. James Biddle Part 1 - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Increase Testosterone Naturally With these Diet And Workout Secrets - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Sector Update: Healthcare - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Signs And Symptoms of Hypogonadism [Last Updated On: March 16th, 2025] [Originally Added On: November 2nd, 2012]
- Auxilium and Pfizer Will Conclude Agreement on XIAPEX® EU Collaboration [Last Updated On: March 16th, 2025] [Originally Added On: November 9th, 2012]
- Repros Therapeutics Inc.(R) Reports Third Quarter 2012 Financial Results [Last Updated On: March 16th, 2025] [Originally Added On: November 14th, 2012]
- hypogonadotropic hypogonadism - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 22nd, 2012]
- Research and Markets: Male Hypogonadism - Pipeline Review, H2 2012 [Last Updated On: March 16th, 2025] [Originally Added On: November 30th, 2012]
- Auxilium Pharmaceuticals, Inc. to Present At The Oppenheimer 23rd Annual Growth Conference [Last Updated On: March 16th, 2025] [Originally Added On: December 8th, 2012]
- Low Testosterone (Hypogonadism) - Part 2 - Video [Last Updated On: March 16th, 2025] [Originally Added On: December 10th, 2012]
- The National Mesothelioma Law Firm of Baron and Budd Reports on a New Drug that Could Improve the Health of ... [Last Updated On: March 16th, 2025] [Originally Added On: December 19th, 2012]
- Hypogonadism ¦ Treatment and Symptoms - Video [Last Updated On: March 16th, 2025] [Originally Added On: March 7th, 2013]
- Research and Markets: Male Hypogonadism Global Clinical Trials Review, H1, 2013 [Last Updated On: March 16th, 2025] [Originally Added On: May 1st, 2013]
- Male hypogonadism Prof Ossama Fouda - Video [Last Updated On: March 16th, 2025] [Originally Added On: May 9th, 2013]
- Low Testosterone (Hypogonadism) - Part 3 - Video [Last Updated On: March 16th, 2025] [Originally Added On: July 2nd, 2013]
- Hypogonadism - what should you do - Video [Last Updated On: March 16th, 2025] [Originally Added On: July 2nd, 2013]
- NURS805 Hypogonadism Lecture - Video [Last Updated On: March 16th, 2025] [Originally Added On: August 16th, 2013]
- Hypogonadism: MedlinePlus Medical Encyclopedia [Last Updated On: March 16th, 2025] [Originally Added On: November 3rd, 2013]
- Hypogonadism - Diseases & Conditions - Medscape Reference [Last Updated On: March 16th, 2025] [Originally Added On: November 10th, 2013]
- Hypogonadotropic hypogonadism - Wikipedia, the free encyclopedia [Last Updated On: March 16th, 2025] [Originally Added On: November 10th, 2013]
- Low Testosterone (Low-T) Normal Levels, Hypogonadism, Symptoms ... [Last Updated On: March 16th, 2025] [Originally Added On: November 15th, 2013]
- HYPOGONADISM - University of Dundee [Last Updated On: March 16th, 2025] [Originally Added On: November 23rd, 2013]
- FAQ - Hypogonadism - MEDICAL DIAGNOSIS AND MEDICINAL PLANTS [Last Updated On: March 16th, 2025] [Originally Added On: November 23rd, 2013]
- Hypogonadism - About.com Men's Health [Last Updated On: March 16th, 2025] [Originally Added On: December 2nd, 2013]
- Exciting medical advances using HRT [Last Updated On: March 16th, 2025] [Originally Added On: December 12th, 2013]
- Male hypogonadism: Symptoms - MayoClinic.com [Last Updated On: March 16th, 2025] [Originally Added On: December 12th, 2013]
- Audio-Digest Foundation Announces the Release of Oncology Volume 04, Issue 16: Highlights from Future Directions ... [Last Updated On: March 16th, 2025] [Originally Added On: December 15th, 2013]
- Hypogonadism - Medscape Reference [Last Updated On: March 16th, 2025] [Originally Added On: December 21st, 2013]
- Hypogonadism [Last Updated On: March 16th, 2025] [Originally Added On: December 23rd, 2013]
- Hypogonadism - HealthCentral [Last Updated On: March 16th, 2025] [Originally Added On: December 24th, 2013]
- Hypogonadism | Medscape - Latest Medical News, Clinical Trials ... [Last Updated On: March 16th, 2025] [Originally Added On: December 30th, 2013]
- Hypogonadism - SharedJourney [Last Updated On: March 16th, 2025] [Originally Added On: January 23rd, 2014]
- Study Finds Potential Heart Risks from Testosterone Therapy [Last Updated On: March 16th, 2025] [Originally Added On: February 3rd, 2014]
- Endocrine Society calls for large-scale studies to evaluate testosterone therapy risks [Last Updated On: March 16th, 2025] [Originally Added On: February 8th, 2014]
- Testosterone Therapy Not Always Good for Older Men [Last Updated On: March 16th, 2025] [Originally Added On: February 11th, 2014]
- Hypogonadism: Types, Causes, & Symptoms Healthline [Last Updated On: March 16th, 2025] [Originally Added On: February 14th, 2014]
- Low Testosterone (Hypogonadism) in Men - Video [Last Updated On: March 16th, 2025] [Originally Added On: February 14th, 2014]
- Hypogonadism : Types, Causes, & Symptoms - Healthline [Last Updated On: March 16th, 2025] [Originally Added On: February 17th, 2014]
- Hypogonadism | Medscape - Latest Medical News, Clinical ... [Last Updated On: March 16th, 2025] [Originally Added On: February 23rd, 2014]
- Endo: FDA Oks AVEED Injection For Treatment Of Adult Men With Hypogonadism [Last Updated On: March 16th, 2025] [Originally Added On: March 6th, 2014]
- Unit Project 1 Hypogonadotropic hypogonadism - Video [Last Updated On: March 16th, 2025] [Originally Added On: March 8th, 2014]
- Update on Endo's Product Portfolio - Analyst Blog [Last Updated On: March 16th, 2025] [Originally Added On: March 11th, 2014]
- Male hypogonadism Symptoms - Diseases and Conditions ... [Last Updated On: March 16th, 2025] [Originally Added On: April 2nd, 2014]
- Hypogonadism: Types, Causes, & Symptoms - Medical ... [Last Updated On: March 16th, 2025] [Originally Added On: April 6th, 2014]
- VLog #127 Frances Explains Hypogonadism. - Video [Last Updated On: March 16th, 2025] [Originally Added On: April 7th, 2014]
- Repros Completes Enrollment for Androxal Study - Analyst Blog [Last Updated On: March 16th, 2025] [Originally Added On: April 16th, 2014]
- Prevalence, Diagnosis and Treatment of Hypogonadism in ... [Last Updated On: March 16th, 2025] [Originally Added On: April 30th, 2014]
- Repros Therapeutics Q2 Loss a Penny Wider than Expected - Analyst Blog [Last Updated On: March 16th, 2025] [Originally Added On: August 12th, 2014]
- Repros Reports Encouraging Late-Stage Data on Androxal - Analyst Blog [Last Updated On: March 16th, 2025] [Originally Added On: August 28th, 2014]
- Repros Therapeutics Analyst Brief Report; Androxal(R) Achieves Superiority in Top Line Analysis by Small Cap Street ... [Last Updated On: March 16th, 2025] [Originally Added On: September 30th, 2014]
- The Wall Street Journal: Repros Therapeutics shares drop on drug application setback [Last Updated On: March 16th, 2025] [Originally Added On: October 18th, 2014]
- Apricus expands development pipeline with in-licensing of US rights for fispemifene [Last Updated On: March 16th, 2025] [Originally Added On: October 21st, 2014]
- Apricus expands development pipeline with the in-licensing of US rights for fispemifene, a phase 2b ready asset, from ... [Last Updated On: March 16th, 2025] [Originally Added On: October 21st, 2014]
- Hypogonadism No Moustache! No Beard!! [Last Updated On: March 16th, 2025] [Originally Added On: October 28th, 2014]
- Male Hypogonadism: Male Reproductive Endocrinology: Merck ... [Last Updated On: March 16th, 2025] [Originally Added On: October 28th, 2014]
- Hypogonadism Wikipedia [Last Updated On: March 16th, 2025] [Originally Added On: October 28th, 2014]
- Urology Care Foundation - Urology A-Z - Low Testosterone [Last Updated On: March 16th, 2025] [Originally Added On: November 3rd, 2014]
- Will Repros (RPRX) Miss Estimates This Earnings Season? - Analyst Blog [Last Updated On: March 16th, 2025] [Originally Added On: November 5th, 2014]
- Hypogonadism in men living with HIV - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 7th, 2014]
- Male Hypogonadism Therapeutic Pipeline Industry Review, H2 2014 - Video [Last Updated On: March 16th, 2025] [Originally Added On: November 7th, 2014]
- Testosterone Deficiency (Hypogonadism) Overview ... [Last Updated On: March 16th, 2025] [Originally Added On: November 23rd, 2014]
- Endo to Acquire Rights to Testosterone Nasal Gel Natesto - Analyst Blog [Last Updated On: March 16th, 2025] [Originally Added On: November 26th, 2014]
- Male hypogonadism pathophysiology - Video [Last Updated On: March 16th, 2025] [Originally Added On: January 14th, 2015]
- Auxilium Announces Results from Special Meeting of Stockholders [Last Updated On: March 16th, 2025] [Originally Added On: January 28th, 2015]
- What is Hypogonadism - Symptoms and Treatment | Hormone ... [Last Updated On: March 16th, 2025] [Originally Added On: January 30th, 2015]
- Male Hypogonadism 1/28/15 - Video [Last Updated On: March 16th, 2025] [Originally Added On: January 31st, 2015]
- Male hypogonadism: symptoms, cause, treatment, risk ... [Last Updated On: March 16th, 2025] [Originally Added On: February 18th, 2015]
Word Count: 1427