While not as severe as the female menopause, the male version is lengthier, usually lasting 15 to 20 years. About 40% of men in their 40s, 50s and 60s experience some degree of lethargy, depression, increased irritability, mood swings, and difficulty in attaining and sustaining erections that characterize andropause.
(Article continues below...)
Concerned or curious about your health? Click below...
The concept of a male andropause has been more controversial than that of the female menopause, with many arguing that it doesn't even exist. Part of the reason for the controversy is that, in contrast to women, men do not have a clear-cut external sign, namely the cessation of menstruation.
A man often begins to experience changes in his body somewhere between the ages of 40 and 55. These bodily changes may be accompanied by changes in attitudes and moods. The aging process alone can not be responsible for this problem as well over 40% of males remain sexually active at 70 years of age and beyond.
Acute andropause in men is relatively uncommon, compared to acute menopause in women, because testicular function declines gradually in most men. There are a number of other causes, however, for acute testicular failure in adult men and these include: viral infections such as mumps, surgical removal of or surgical injury to the testes and male reproductive tract, diseases when the immune system attacks and destroys the testes such as variations of systemic lupus erythematosis, subtle genetic abnormalities which permit normal adult development but lead to premature testicular failure, generalized vascular diseases such as diabetes, chemotherapy, and pituitary tumors (rare).
The second form of this syndrome, while more common, is more insidious since it occurs gradually. It is often confused with male midlife psychological adjustment disorders because it exactly mimics depression in midlife men. Some known contributors to this condition are excessive alcohol consumption, smoking, hypertension, prescription and non-prescription medications, poor diet, lack of exercise, poor circulation, and psychological problems.
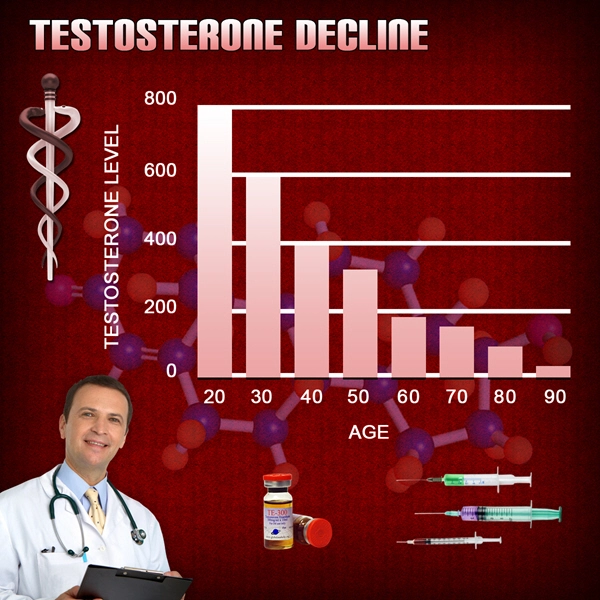
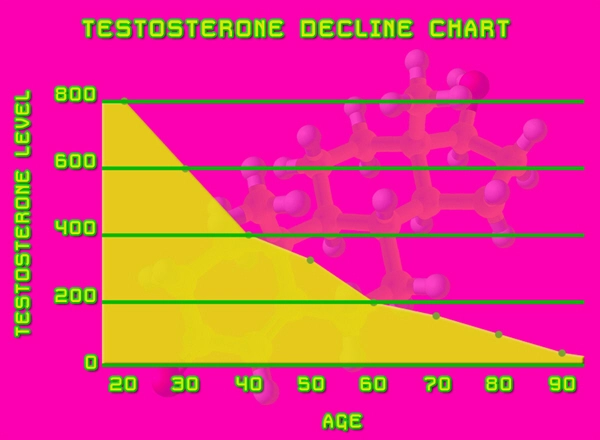
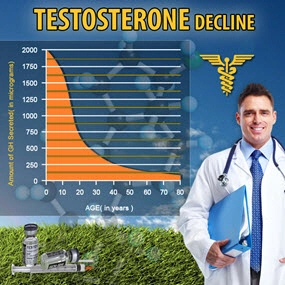
Male hormones decline gradually. Testosterone (from the testes), human growth hormone (from the pituitary), and DHEA and androstenedione (from the adrenal gland) levels all begin to drop. For many men this does not occur until their 60s or 70s but there are others where it occurs much earlier. In addition, there are proteins in the blood which bind testosterone into a biologically inactive form sex hormone binding proteins or globulins. Their levels can rise in response to many conditions including medical disorders and exposure to other hormones such as phytoestrogens (estrogens derived from plant sources such as soy) and environmental estrogen-like compounds (pesticides, hormones used in agribusiness to produce fatter animals, etc.) As an example, there is some data suggesting that men on low fat or vegetarian diets have lower testosterone levels. The overall effect of rising sex hormone binding proteins is that there is less bio-available testosterone.
Typical symptoms include:
This list sounds a little similar to women in menopause because it is the same condition. The relationship between the ovaries, estrogen, the brain, and the pituitary are the same as the relationship between the testes, testosterone, the brain, and the pituitary.
The diagnosis is simple measuring either free testosterone blood levels or computing the Free Androgen Index (FAI) which is [total testosterone x 100 / sex hormone binding globulin]. There is some controversy as to what level of total blood testosterone in men is normal with low end values ranging from 250-400ng/dl. Free testosterone in men should be well within the range of 300-1100ng/dl with the FAI between 70-100%. At a FAI of less than 50%, symptoms of andropause appear.
Risks of replacement therapy. Though often suggested, there is no evidence in the medical literature that testosterone replacement therapy increases the risk of prostate cancer. Men using synthetic testosterone supplementation should have their serum lipids carefully evaluated and rechecked periodically. Using a natural testosterone is safer than using a synthetic form, but may require the transdermal route of administration.
As a general principle, whenever any hormone is administered, the gland which normally produces it ceases to function and recovery when therapy stops can be variable. Patients with borderline low testosterone levels may be committing themselves to lifelong therapy if they start with testosterone replacement.
Benefits of replacement therapy There is no doubt that the administration of testosterone to men with true testosterone deficiency will improve their health and sense of well being. The symptoms listed above should disappear. Unfortunately impotence, or the inability to sustain and erection, does not respond well to testosterone therapy except perhaps in men with severe hormone deficiencies. This comprises approximately 8-16% of men presenting themselves to physicians with erectile disorders. There is no evidence that administering testosterone to men with borderline low testosterone levels will improve sexual functioning, although libido may be enhanced.
Here is the original post:
Andropause/Male Menopause - Symptoms and Diagnosis
Contact Us Today For A Free Consultation

- Andropause Symptoms Treatment - Fixing Male Menopause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Andropause: Male Menopause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- About Andropause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- MALE MENOPAUSE, MANOPAUSE, OR ANDROPAUSE? - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Andropause Menopause Symptoms and Solutions Testosterone - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Treatments for Male Menopause/Andropause/Manopause/Testosterone Deficiency - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- What is testosterone deficiency syndrome/male menopause/.andropause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Testosterone Deficiency Syndrome/Andropause - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- John Crisler DO - Andropause [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Menopause/Andropause [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Male Andropause: Part 2 - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Dr. Steven Jepson discusses Andropause - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Maturitas publishes clinical guide on low-dose vaginal estrogens for vaginal atrophy [Last Updated On: January 10th, 2018] [Originally Added On: September 13th, 2012]
- Testosterone Deficiency in Men - Andropause Symptoms and Treatment - Video [Last Updated On: January 4th, 2025] [Originally Added On: November 2nd, 2012]
- Andropause - The Male Menopause - Video [Last Updated On: January 3rd, 2025] [Originally Added On: November 2nd, 2012]
- SA STGEC ~ Ad Hoc Talk: Andropause (2006) - Video [Last Updated On: January 4th, 2025] [Originally Added On: November 2nd, 2012]
- The Cosmetic Medic Stamford CT - Video [Last Updated On: January 5th, 2025] [Originally Added On: November 2nd, 2012]
- Testosterone Roundtable -- Overview of Low Testosterone (Part 1) - Video [Last Updated On: January 5th, 2025] [Originally Added On: November 2nd, 2012]
- Naturally Increase Testosterone Levels - Video [Last Updated On: February 8th, 2025] [Originally Added On: November 26th, 2012]
- Patients Medical Welcomes Dr. Marcia A. Harris, Holistic Gynecologist and Anti-Aging Physician [Last Updated On: June 7th, 2025] [Originally Added On: December 2nd, 2012]
- ALCAT Pioneer, Roger Deutsch, to Address "Food Induced Inflammation and Aging" at Vienna's Prestigious December ... [Last Updated On: June 8th, 2025] [Originally Added On: December 5th, 2012]
- Andropause: Changes in Aging Men - Video [Last Updated On: February 19th, 2025] [Originally Added On: December 10th, 2012]
- Rhein Test Kit - Avante Medical Center - Video [Last Updated On: February 19th, 2025] [Originally Added On: December 10th, 2012]
- AM Northwest Appearance - Andropause - Video [Last Updated On: February 19th, 2025] [Originally Added On: December 10th, 2012]
- Lessons in Menopause for Men - Video [Last Updated On: December 15th, 2012] [Originally Added On: December 15th, 2012]
- AAG Health Publishes Testosterone and HGH Discussion-Blog [Last Updated On: June 11th, 2025] [Originally Added On: December 26th, 2012]
- Understanding Andropause: Erectile Dysfunction - Part Two - Video [Last Updated On: February 26th, 2013] [Originally Added On: February 26th, 2013]
- Airing March 2 and 3: BBC World News 30-Minute Segment on Andropause/Aging with Dr. Jeff Life, Healthy Aging Expert ... [Last Updated On: February 26th, 2025] [Originally Added On: February 28th, 2013]
- Andropause - Great Android App For Men - Vigor - Stamina - Video [Last Updated On: February 28th, 2013] [Originally Added On: February 28th, 2013]
- Eastday-Survey finds 1m locals suffer from andropause [Last Updated On: August 23rd, 2025] [Originally Added On: May 22nd, 2013]
- What Is Andropause?Diagnosis,Symptoms,Treatment [Last Updated On: March 11th, 2025] [Originally Added On: July 2nd, 2013]
- Andropause - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Andropause Glossary - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Andropause Symptoms - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Understanding Andropause: Erectile Dysfunction - Part One - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Understanding Andropause - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Andropause video - Video [Last Updated On: July 8th, 2013] [Originally Added On: July 8th, 2013]
- ANDROPAUSE SOLUTION "OSS-TEST" TOP BEST NATURAL TESTOSTERONE BOOSTER - Video [Last Updated On: August 3rd, 2013] [Originally Added On: August 3rd, 2013]
- Natural relief for andropause [Last Updated On: December 2nd, 2017] [Originally Added On: October 10th, 2013]
- Andropause - Causes, Symptoms, Treatment, Diagnosis - Seniors ... [Last Updated On: January 7th, 2018] [Originally Added On: November 3rd, 2013]
- Andropause - Causes, Symptoms, Treatment, Diagnosis - Men's Health ... [Last Updated On: December 31st, 2017] [Originally Added On: November 3rd, 2013]
- Andropause Specialist [Last Updated On: January 21st, 2018] [Originally Added On: November 10th, 2013]
- Understanding Andropause [Last Updated On: October 24th, 2015] [Originally Added On: November 10th, 2013]
- Andropause - Causes, Symptoms, Treatment, Diagnosis - Men's ... [Last Updated On: January 20th, 2018] [Originally Added On: November 18th, 2013]
- Andropause | Male Menopause | Male Menopause Symptoms | Male ... [Last Updated On: November 25th, 2018] [Originally Added On: November 18th, 2013]
- Symptoms of andropause - Men's health [Last Updated On: November 25th, 2018] [Originally Added On: November 21st, 2013]
- Andropause In Men [Last Updated On: December 9th, 2017] [Originally Added On: November 23rd, 2013]
- Andropause - Male Menopause - Androgen Replacement Therapy [Last Updated On: January 13th, 2018] [Originally Added On: November 25th, 2013]
- Andropause 2013 - Reviewed and Ranked - Independent Reviews on ... [Last Updated On: March 30th, 2025] [Originally Added On: November 25th, 2013]
- Andropause, Facts, Symptoms, Diagnosis, Testosterone Treatment [Last Updated On: January 18th, 2018] [Originally Added On: November 27th, 2013]
- Symptoms of Andropause (Male Menopause): Low Testosterone, Low ... [Last Updated On: December 13th, 2017] [Originally Added On: November 27th, 2013]
- Discovery Health "Andropause: Dealing With Male Menopause" [Last Updated On: December 5th, 2017] [Originally Added On: November 27th, 2013]
- Global Toronto's News at Noon Andropause aka "manopause" - Video [Last Updated On: November 27th, 2013] [Originally Added On: November 27th, 2013]
- San Diego Dermatologist Discusses Male Menopause | Andropause Expert in San Diego - Video [Last Updated On: December 7th, 2017] [Originally Added On: December 9th, 2013]
- The American Academy of Anti-Aging Medicine (A4M) Concludes Largest Event in Anti-Aging, Regenerative and Aesthetic ... [Last Updated On: April 5th, 2025] [Originally Added On: December 19th, 2013]
- Andropause Symptoms - Male Menopause Symptoms [Last Updated On: December 16th, 2017] [Originally Added On: December 27th, 2013]
- What Is Andropause? | eHow - eHow | How to Videos, Articles ... [Last Updated On: January 20th, 2018] [Originally Added On: December 30th, 2013]
- Drug companies are pushing that new-man feeling Low T, high stakes [Last Updated On: April 10th, 2025] [Originally Added On: January 16th, 2014]
- Andropause - Male Menopause - Androgen Replacement Therapy ... [Last Updated On: December 24th, 2017] [Originally Added On: January 16th, 2014]
- Male Menopause Symptoms, Treatments, Causes, and More [Last Updated On: January 15th, 2018] [Originally Added On: January 16th, 2014]
- Can you reverse the aging process? [Last Updated On: April 11th, 2025] [Originally Added On: January 17th, 2014]
- Yourwellness Magazine Explores Male Menopause [Last Updated On: April 12th, 2025] [Originally Added On: January 19th, 2014]
- Antiaging Medicine and Research, India Will Highlight “Hormones and Aging in Medical Practice” During 5th Indomedicon ... [Last Updated On: April 14th, 2025] [Originally Added On: January 24th, 2014]
- Care needed when controlling cholesterol [Last Updated On: October 23rd, 2020] [Originally Added On: January 27th, 2014]
- Symptoms of Andropause (Male Menopause): Low Testosterone ... [Last Updated On: October 11th, 2020] [Originally Added On: January 30th, 2014]
- Antiaging Medicine and Research, India Will Highlight Hormones and Aging in Medical Practice During 5th Indomedicon ... [Last Updated On: October 24th, 2020] [Originally Added On: January 31st, 2014]
- The truth about low testosterone and 'male menopause' [Last Updated On: October 31st, 2020] [Originally Added On: January 31st, 2014]
- Surge or shrink [Last Updated On: November 1st, 2020] [Originally Added On: February 11th, 2014]
- How Does Andropause Affect Men? - Video [Last Updated On: November 10th, 2020] [Originally Added On: February 14th, 2014]
- Andropause | Male Menopause | Male Menopause Symptoms ... [Last Updated On: November 25th, 2018] [Originally Added On: February 15th, 2014]
- NuMale Medical - Low Testosterone -- Andropause - Video [Last Updated On: October 21st, 2020] [Originally Added On: February 21st, 2014]
- Boost Your Sex Drive: Solutions For Impotence, Erectile Dysfunction And Low Libido [Last Updated On: September 18th, 2025] [Originally Added On: February 27th, 2014]
- HowStuffWorks "Andropause: Dealing With Male Menopause" [Last Updated On: October 16th, 2020] [Originally Added On: March 7th, 2014]
- The Truth About Andropause: Male Menopause - Explained by Hormone Expert, Dr. Ken G. Knott, MD - Video [Last Updated On: November 20th, 2020] [Originally Added On: March 7th, 2014]
- What Is Andropause? It's Symptoms In Men & Treatment ... [Last Updated On: November 11th, 2020] [Originally Added On: March 14th, 2014]
- Andropause Low Testosterone A Drug Free Natural Approach UnitedMulticare com - Video [Last Updated On: October 9th, 2020] [Originally Added On: March 15th, 2014]
- Low Testosterone (Andropause). What is it? - Video [Last Updated On: October 30th, 2020] [Originally Added On: March 15th, 2014]
- Male menopause is a reality [Last Updated On: October 13th, 2020] [Originally Added On: March 24th, 2014]
- Anatomy Menopause Andropause - Video [Last Updated On: March 25th, 2014] [Originally Added On: March 25th, 2014]
- Menopause & Andropause - Video [Last Updated On: November 7th, 2020] [Originally Added On: March 30th, 2014]
Word Count: 802