Hypogonadism is the term for any condition which causes sex hormones to be produced at levels that are inadequate for normal and healthy function.
In males, Hypogonadism is also known as Low-T or Testosterone Deficiency. Dependent upon the age at which Hypogonadism becomes a health issue, the symptoms can be dramatically different.
Healthy sex hormone production is absolutely necessary for the development of secondary sexual characteristics during puberty, and if Testosterone or Estrogen Levels are too low, this can lead to delayed puberty or underdevelopment.
Video Link: https://vimeo.com/291609390
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
In adulthood, Hypogonadism affects physiological function rather than development. Testosterone is vitally important to both health and sexual function in men.
In women, Estrogen is necessary for the menstrual cycle and normal fertility. In both sexes, Testosterone is directly associated with sexual desire and performance. If a man doesn't produce enough Testosterone, libido suffers, erectile function diminishes, and fertility falls dramatically.
Treatments options for Hypogonadism depend on the underlying cause of Sex Hormone Deficiency but usually revolve around effective use of Testosterone Replacement Therapy or Clomiphene Citrate.
Primary Hypogonadism in Men
In men, Primary Hypogonadism is a condition in which the testes are unable to adequately produce Testosterone in order to meet the physiological requirements of the body.
Primary Hypogonadism is also known as hypogonadotropic Hypogonadism. The word Hypogonadism refers to general Testosterone Deficiency in males.
Hypergonadotropic refers to a symptom of this form of Testosterone Deficiency in which the brain signals for the elevated production of Testosterone Precursors in order to compensate for inhibited Testosterone Production.
Gonadotropic refers to hormones intended to stimulate the production of sex hormones. In both sexes, the most significant Gonadotropic Hormones are Luteinizing Hormone and Follicle-Stimulating Hormone.
Causes of Primary Hypogonadism
Primary Hypogonadism is actually the rarest form of Testosterone Deficiency, because aging is the number one cause of Low-T, and occurs whether the testes are healthy enough for Testosterone and Sperm Production.
are healthy enough for Testosterone and Sperm Production.
Primary Hypogonadism has many causes, resulting from either damage to the testes or underdevelopment of the Testes.
Prenatally, Genetic disorders, and congenital defects are among the causes of Primary Hypogonadism, and one of the most common of these disorders is Klinefelter Syndrome.
Undescended or partially descended Testicles can also lead to Testosterone Deficiency, and in some cases may require surgery to fix.
Among adults, physical damage to the testes is the general cause of Primary Hypogonadism, and this damage can be the result of several different factors. Cancer treatment can significantly damage the testes, leading to inhibited Testosterone and sperm production.
Excess iron levels (known as hemochromatosis) can lead to partial or total failure of the testes (as well as the pituitary gland). Diseases such as the Mumps can also significantly impact the normal and healthy function of the Testicles.
Secondary Hypogonadism in Men
Secondary Hypogonadism is a form of Hormone Deficiency in which the sex organs are still perfectly capable of producing sex hormones, but signaling for the production of those Hormones has dropped to levels that lead to Sex Hormone Deficiency.
This is the most common cause of Testosterone Deficiency in men. Secondary Hypogonadism is also referred to as Normogonadotropic Hypogonadism.
Men suffering from Secondary Hypogonadism have issues producing both Testosterone and Sperm. The severity of these issues is directly correlated with the severity of the patient's Low-T.
Testosterone is produced as a response to stimulation by Luteinizing Hormone  released by cells in the Anterior Pituitary Gland known as Gonadotropic Cells. Less Luteinizing Hormone means that the testes secrete less Testosterone.
released by cells in the Anterior Pituitary Gland known as Gonadotropic Cells. Less Luteinizing Hormone means that the testes secrete less Testosterone.
Whether a man has Primary or Secondary Hypogonadism, he will likely have issues with sperm production. Because of underlying differences between the two forms of Hypogonadism, men with Secondary Hypogonadism are more likely to experience significant Testosterone Deficiency than their counterparts.
This is because the cells responsible for the production of Semen are more sensitive than the cells associated with the production of Testosterone, which makes them more prone to damage and malfunction.
In many cases, men with Primary Hypogonadism are more than capable of producing Testosterone but have a significantly suppressed or total inability to produce sperm.
Causes of Secondary Hypogonadism
Like Primary Hypogonadism, Secondary Hypogonadism can also be the result of congenital issues, one of which is Kallman Syndrome. Damage to the pituitary gland from cancer treatment and tumor extraction can also lead to Secondary Hypogonadism, as well as the development of the tumor itself.
Obesity is well-known for suppressing Testosterone production by increasing Estrogen Levels in the male bloodstream. Any condition which leads to severe inflammation which directly or indirectly impacts the hypothalamus or pituitary gland can also lead to Secondary Hypogonadism.
Of course, one of the most common causes of symptomatic Secondary Hypogonadism is aging, itself.
Age-Associated Hypogonadism in Men
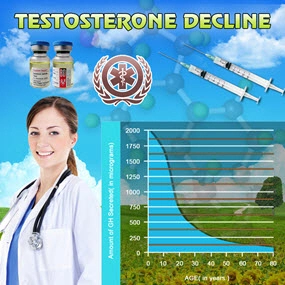
The most common form of Hypogonadism by far is Age-Associated Hypogonadism. The physiological process by which this condition occurs is known as Andropause. Andropause can be most easily understood as the male counterpart to menopause.
Both are conditions that lead to significant changes in metabolism, as well as physical and psychological function, and both are directly the result of a decline in gender-associated Hormone Levels (Testosterone in men, Estradiol in women).
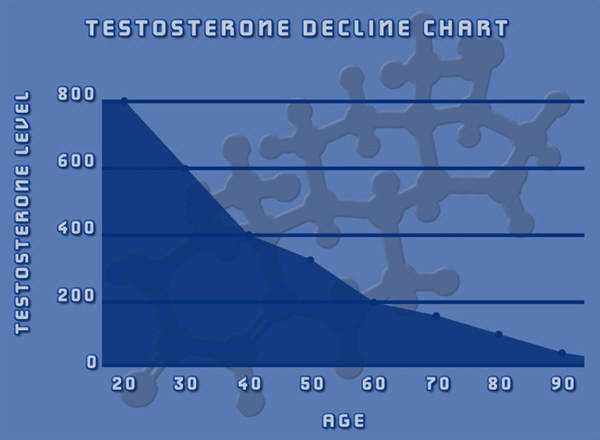
There are two major differences between Andropause and Menopause. First, Andropause is the result of a slow decline in Testosterone that occurs over the course of many years, which becomes more rapid during the forties and fifties.
Menopause is a sudden change that occurs at the end of a woman's reproductive life. Second, men continue to produce Testosterone (albeit at lesser concentrations over time) throughout their lifespan, whereas Menopause is a cessation of the production of Estradiol.
Secondary Hypogonadism and Fertility
Normogonadotropic Hypogonadism refers to Sex Hormone Deficiency in which Follicle-Stimulating Hormone and Luteinizing Hormones are produced at normal levels, but Testosterone Levels in the bloodstream are still abnormally low.
For men suffering from fertility issues related to Normogonadotropic Hypogonadism, Clomiphene Citrate is one of the most popular methods to stimulate an increase in Testosterone Levels in order to spur the pr oduction of sperm in order to increase the odds of fertilization.
oduction of sperm in order to increase the odds of fertilization.
Clomiphene Citrate prevents Estrogen from suppressing Luteinizing Hormone and Follicle-Stimulating Hormone production, increasing Gonadotropin production, and encouraging normalized secretion of Testosterone and manufacture of sperm.
Contact Us Today For A Free Consultation

- Andropause Symptoms Treatment - Fixing Male Menopause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Andropause: Male Menopause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- About Andropause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- MALE MENOPAUSE, MANOPAUSE, OR ANDROPAUSE? - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Andropause Menopause Symptoms and Solutions Testosterone - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Treatments for Male Menopause/Andropause/Manopause/Testosterone Deficiency - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- What is testosterone deficiency syndrome/male menopause/.andropause - Video [Last Updated On: November 25th, 2024] [Originally Added On: July 12th, 2012]
- Testosterone Deficiency Syndrome/Andropause - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- John Crisler DO - Andropause [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Menopause/Andropause [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Male Andropause: Part 2 - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Dr. Steven Jepson discusses Andropause - Video [Last Updated On: December 20th, 2024] [Originally Added On: July 12th, 2012]
- Maturitas publishes clinical guide on low-dose vaginal estrogens for vaginal atrophy [Last Updated On: January 10th, 2018] [Originally Added On: September 13th, 2012]
- Testosterone Deficiency in Men - Andropause Symptoms and Treatment - Video [Last Updated On: January 4th, 2025] [Originally Added On: November 2nd, 2012]
- Andropause - The Male Menopause - Video [Last Updated On: January 3rd, 2025] [Originally Added On: November 2nd, 2012]
- SA STGEC ~ Ad Hoc Talk: Andropause (2006) - Video [Last Updated On: January 4th, 2025] [Originally Added On: November 2nd, 2012]
- The Cosmetic Medic Stamford CT - Video [Last Updated On: January 5th, 2025] [Originally Added On: November 2nd, 2012]
- Testosterone Roundtable -- Overview of Low Testosterone (Part 1) - Video [Last Updated On: January 5th, 2025] [Originally Added On: November 2nd, 2012]
- Naturally Increase Testosterone Levels - Video [Last Updated On: February 8th, 2025] [Originally Added On: November 26th, 2012]
- Patients Medical Welcomes Dr. Marcia A. Harris, Holistic Gynecologist and Anti-Aging Physician [Last Updated On: June 7th, 2025] [Originally Added On: December 2nd, 2012]
- ALCAT Pioneer, Roger Deutsch, to Address "Food Induced Inflammation and Aging" at Vienna's Prestigious December ... [Last Updated On: June 8th, 2025] [Originally Added On: December 5th, 2012]
- Andropause: Changes in Aging Men - Video [Last Updated On: February 19th, 2025] [Originally Added On: December 10th, 2012]
- Rhein Test Kit - Avante Medical Center - Video [Last Updated On: February 19th, 2025] [Originally Added On: December 10th, 2012]
- AM Northwest Appearance - Andropause - Video [Last Updated On: February 19th, 2025] [Originally Added On: December 10th, 2012]
- Lessons in Menopause for Men - Video [Last Updated On: December 15th, 2012] [Originally Added On: December 15th, 2012]
- AAG Health Publishes Testosterone and HGH Discussion-Blog [Last Updated On: June 11th, 2025] [Originally Added On: December 26th, 2012]
- Understanding Andropause: Erectile Dysfunction - Part Two - Video [Last Updated On: February 26th, 2013] [Originally Added On: February 26th, 2013]
- Airing March 2 and 3: BBC World News 30-Minute Segment on Andropause/Aging with Dr. Jeff Life, Healthy Aging Expert ... [Last Updated On: February 26th, 2025] [Originally Added On: February 28th, 2013]
- Andropause - Great Android App For Men - Vigor - Stamina - Video [Last Updated On: February 28th, 2013] [Originally Added On: February 28th, 2013]
- Eastday-Survey finds 1m locals suffer from andropause [Last Updated On: August 23rd, 2025] [Originally Added On: May 22nd, 2013]
- What Is Andropause?Diagnosis,Symptoms,Treatment [Last Updated On: March 11th, 2025] [Originally Added On: July 2nd, 2013]
- Andropause - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Andropause Glossary - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Andropause Symptoms - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Understanding Andropause: Erectile Dysfunction - Part One - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Understanding Andropause - Video [Last Updated On: July 2nd, 2013] [Originally Added On: July 2nd, 2013]
- Andropause video - Video [Last Updated On: July 8th, 2013] [Originally Added On: July 8th, 2013]
- ANDROPAUSE SOLUTION "OSS-TEST" TOP BEST NATURAL TESTOSTERONE BOOSTER - Video [Last Updated On: August 3rd, 2013] [Originally Added On: August 3rd, 2013]
- Natural relief for andropause [Last Updated On: December 2nd, 2017] [Originally Added On: October 10th, 2013]
- Andropause - Causes, Symptoms, Treatment, Diagnosis - Seniors ... [Last Updated On: January 7th, 2018] [Originally Added On: November 3rd, 2013]
- Andropause - Causes, Symptoms, Treatment, Diagnosis - Men's Health ... [Last Updated On: December 31st, 2017] [Originally Added On: November 3rd, 2013]
- Andropause Specialist [Last Updated On: January 21st, 2018] [Originally Added On: November 10th, 2013]
- Understanding Andropause [Last Updated On: October 24th, 2015] [Originally Added On: November 10th, 2013]
- Andropause - Causes, Symptoms, Treatment, Diagnosis - Men's ... [Last Updated On: January 20th, 2018] [Originally Added On: November 18th, 2013]
- Andropause | Male Menopause | Male Menopause Symptoms | Male ... [Last Updated On: November 25th, 2018] [Originally Added On: November 18th, 2013]
- Symptoms of andropause - Men's health [Last Updated On: November 25th, 2018] [Originally Added On: November 21st, 2013]
- Andropause In Men [Last Updated On: December 9th, 2017] [Originally Added On: November 23rd, 2013]
- Andropause - Male Menopause - Androgen Replacement Therapy [Last Updated On: January 13th, 2018] [Originally Added On: November 25th, 2013]
- Andropause 2013 - Reviewed and Ranked - Independent Reviews on ... [Last Updated On: March 30th, 2025] [Originally Added On: November 25th, 2013]
- Andropause, Facts, Symptoms, Diagnosis, Testosterone Treatment [Last Updated On: January 18th, 2018] [Originally Added On: November 27th, 2013]
- Symptoms of Andropause (Male Menopause): Low Testosterone, Low ... [Last Updated On: December 13th, 2017] [Originally Added On: November 27th, 2013]
- Discovery Health "Andropause: Dealing With Male Menopause" [Last Updated On: December 5th, 2017] [Originally Added On: November 27th, 2013]
- Global Toronto's News at Noon Andropause aka "manopause" - Video [Last Updated On: November 27th, 2013] [Originally Added On: November 27th, 2013]
- San Diego Dermatologist Discusses Male Menopause | Andropause Expert in San Diego - Video [Last Updated On: December 7th, 2017] [Originally Added On: December 9th, 2013]
- The American Academy of Anti-Aging Medicine (A4M) Concludes Largest Event in Anti-Aging, Regenerative and Aesthetic ... [Last Updated On: April 5th, 2025] [Originally Added On: December 19th, 2013]
- Andropause Symptoms - Male Menopause Symptoms [Last Updated On: December 16th, 2017] [Originally Added On: December 27th, 2013]
- What Is Andropause? | eHow - eHow | How to Videos, Articles ... [Last Updated On: January 20th, 2018] [Originally Added On: December 30th, 2013]
- Drug companies are pushing that new-man feeling Low T, high stakes [Last Updated On: April 10th, 2025] [Originally Added On: January 16th, 2014]
- Andropause - Male Menopause - Androgen Replacement Therapy ... [Last Updated On: December 24th, 2017] [Originally Added On: January 16th, 2014]
- Male Menopause Symptoms, Treatments, Causes, and More [Last Updated On: January 15th, 2018] [Originally Added On: January 16th, 2014]
- Can you reverse the aging process? [Last Updated On: April 11th, 2025] [Originally Added On: January 17th, 2014]
- Yourwellness Magazine Explores Male Menopause [Last Updated On: April 12th, 2025] [Originally Added On: January 19th, 2014]
- Antiaging Medicine and Research, India Will Highlight “Hormones and Aging in Medical Practice” During 5th Indomedicon ... [Last Updated On: April 14th, 2025] [Originally Added On: January 24th, 2014]
- Care needed when controlling cholesterol [Last Updated On: October 23rd, 2020] [Originally Added On: January 27th, 2014]
- Symptoms of Andropause (Male Menopause): Low Testosterone ... [Last Updated On: October 11th, 2020] [Originally Added On: January 30th, 2014]
- Antiaging Medicine and Research, India Will Highlight Hormones and Aging in Medical Practice During 5th Indomedicon ... [Last Updated On: October 24th, 2020] [Originally Added On: January 31st, 2014]
- The truth about low testosterone and 'male menopause' [Last Updated On: October 31st, 2020] [Originally Added On: January 31st, 2014]
- Surge or shrink [Last Updated On: November 1st, 2020] [Originally Added On: February 11th, 2014]
- How Does Andropause Affect Men? - Video [Last Updated On: November 10th, 2020] [Originally Added On: February 14th, 2014]
- Andropause | Male Menopause | Male Menopause Symptoms ... [Last Updated On: November 25th, 2018] [Originally Added On: February 15th, 2014]
- NuMale Medical - Low Testosterone -- Andropause - Video [Last Updated On: October 21st, 2020] [Originally Added On: February 21st, 2014]
- Boost Your Sex Drive: Solutions For Impotence, Erectile Dysfunction And Low Libido [Last Updated On: September 18th, 2025] [Originally Added On: February 27th, 2014]
- HowStuffWorks "Andropause: Dealing With Male Menopause" [Last Updated On: October 16th, 2020] [Originally Added On: March 7th, 2014]
- The Truth About Andropause: Male Menopause - Explained by Hormone Expert, Dr. Ken G. Knott, MD - Video [Last Updated On: November 20th, 2020] [Originally Added On: March 7th, 2014]
- What Is Andropause? It's Symptoms In Men & Treatment ... [Last Updated On: November 11th, 2020] [Originally Added On: March 14th, 2014]
- Andropause Low Testosterone A Drug Free Natural Approach UnitedMulticare com - Video [Last Updated On: October 9th, 2020] [Originally Added On: March 15th, 2014]
- Low Testosterone (Andropause). What is it? - Video [Last Updated On: October 30th, 2020] [Originally Added On: March 15th, 2014]
- Male menopause is a reality [Last Updated On: October 13th, 2020] [Originally Added On: March 24th, 2014]
- Anatomy Menopause Andropause - Video [Last Updated On: March 25th, 2014] [Originally Added On: March 25th, 2014]
- Menopause & Andropause - Video [Last Updated On: November 7th, 2020] [Originally Added On: March 30th, 2014]
Word Count: 1044