Introduction
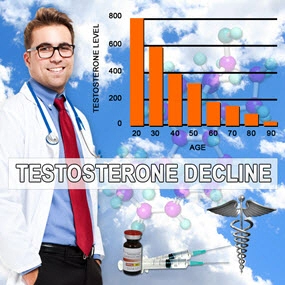
Testosterone, a primary male sex hormone, plays a crucial role in various physiological processes, including muscle mass, bone density, and overall metabolic health. Recent studies have begun to explore the impact of testosterone on respiratory health, particularly in American males. This article delves into a pulmonary study that utilized spirometry tests to assess the effects of low testosterone on lung function, offering valuable insights into the respiratory implications of hormonal imbalances.
Background and Significance
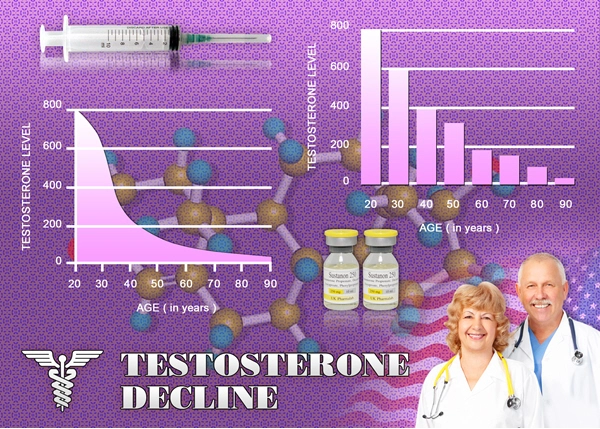
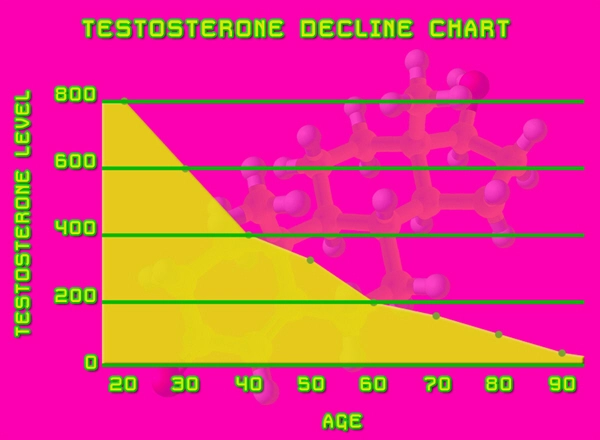
Low testosterone, or hypogonadism, is a prevalent condition among American males, affecting approximately 2.1% of men aged 40 to 79. While the condition is well-known for its impact on sexual health and muscle mass, its effects on respiratory function are less understood. Spirometry, a common pulmonary function test, measures lung capacity and airflow, providing a quantitative assessment of respiratory health. This study aimed to bridge the gap in understanding by examining the correlation between low testosterone levels and spirometry results.
Methodology
The study involved 500 American males aged 40 to 79, divided into two groups: those with normal testosterone levels and those diagnosed with hypogonadism. Participants underwent spirometry tests to measure Forced Vital Capacity (FVC), Forced Expiratory Volume in one second (FEV1), and the FEV1/FVC ratio. Blood samples were also collected to confirm testosterone levels.
Results and Findings
The results revealed significant differences in lung function between the two groups. Men with low testosterone exhibited lower FVC and FEV1 values compared to those with normal testosterone levels. The FEV1/FVC ratio, an indicator of obstructive lung disease, was also lower in the hypogonadism group, suggesting a potential link between low testosterone and impaired respiratory function.
Discussion
The findings of this study suggest that low testosterone may contribute to reduced lung capacity and airflow, potentially increasing the risk of respiratory conditions such as chronic obstructive pulmonary disease (COPD). The exact mechanisms behind this association are not fully understood but may involve testosterone's influence on muscle strength, including the respiratory muscles.
Implications for American Males
For American males, these findings underscore the importance of monitoring testosterone levels, not only for sexual and metabolic health but also for respiratory well-being. Men with hypogonadism may benefit from testosterone replacement therapy (TRT) to improve lung function and reduce the risk of respiratory complications. However, further research is needed to confirm these benefits and establish optimal treatment protocols.
Clinical Recommendations
Healthcare providers should consider assessing testosterone levels in male patients presenting with respiratory symptoms, particularly those with risk factors for hypogonadism. Routine spirometry tests may be warranted for men with low testosterone to monitor lung function and guide treatment decisions.
Limitations and Future Research
While this study provides valuable insights, it has limitations, including its cross-sectional design and the potential influence of confounding factors such as smoking and obesity. Future research should employ longitudinal studies to assess the long-term effects of low testosterone on lung function and explore the potential benefits of TRT in improving respiratory health.
Conclusion
This pulmonary study highlights the significant impact of low testosterone on respiratory health and lung function in American males. By utilizing spirometry tests, researchers have uncovered a potential link between hypogonadism and reduced lung capacity, emphasizing the need for comprehensive hormonal assessments in men with respiratory symptoms. As the understanding of testosterone's role in pulmonary health continues to evolve, American males and their healthcare providers must remain vigilant in monitoring and addressing hormonal imbalances to optimize respiratory well-being.
Contact Us Today For A Free Consultation

- Environmental Toxins and Testosterone: Impacts and Mitigation Strategies for American Men [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- Low Testosterone in American Males: Symptoms, Causes, and Treatment Options [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Low Testosterone's Impact on Muscle Mass and Strength in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Vitamin D's Role in Managing Low Testosterone in American Men: A Comprehensive Review [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Chronic Illness Impact on Low Testosterone in American Males: Management Strategies [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Managing Low Testosterone in Aging Men: Symptoms, Treatments, and Lifestyle Strategies [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Economic Burden of Low Testosterone on American Healthcare System [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Low Testosterone and Diabetes: Dual Challenges Impacting American Men's Health [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Alcohol Consumption and Its Impact on Testosterone Levels in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Zinc's Role in Boosting Testosterone Levels in American Men: A Comprehensive Review [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Low Testosterone and Mood Disorders: Impact and Management in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Low Testosterone in American Men: Symptoms, Diagnosis, and Treatment Strategies [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Smoking's Impact on Testosterone Levels in American Men: Risks and Recovery [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Low Testosterone's Impact on Osteoporosis Risk in American Men: Detection and Management [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone and Prostate Health: Risks, Therapy, and Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone and Hair Loss: Understanding the Link and Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone's Impact on Cognitive Function in American Men: Insights and Interventions [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Shift Work's Impact on Testosterone Levels in American Men: Health Implications and Mitigation [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Low Testosterone's Impact on Immune Health in American Males: Insights and Management [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Optimizing Testosterone Levels: Dietary Strategies for American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Low Testosterone in American Men: Symptoms, Impact, and Treatment Options [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Environmental Estrogens: A Hidden Cause of Low Testosterone in American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Low Testosterone's Impact on Skin Health in American Men: Causes and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Weight Loss Boosts Testosterone: A Guide for American Males with Low T [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Herbal Supplements for Low Testosterone: Benefits, Limitations, and Efficacy in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Managing Low Testosterone in Aging Men: Symptoms, Treatments, and Lifestyle Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone and Heart Disease: Risks, Mechanisms, and Management in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Chronic Stress Impact on Testosterone Levels in American Men: Causes and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone's Impact on Emotional Wellbeing in American Men: Insights and Guidance [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone and Depression: Understanding the Link and Its Impact on American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Sleep Apnea's Impact on Testosterone Levels in American Males: Insights and Solutions [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Medications Impacting Testosterone Levels: Insights for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Low Testosterone and Metabolic Syndrome: Implications for American Men's Health [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Chronic Pain's Impact on Testosterone Levels in American Males: A Comprehensive Analysis [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Genetic Factors in Low Testosterone Among American Males: Insights and Implications [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone Linked to Increased Thyroid Disorder Risk in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone and Insulin Resistance: Exploring the Link in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Exercise Boosts Testosterone: A Guide for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone and Libido: Impacts, Diagnosis, and Treatment for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Low Testosterone's Impact on Body Composition in American Males: Challenges and Management [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Low Testosterone and Skin Health: Dermatological Impacts and Management in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Chronic Inflammation and Low Testosterone: Strategies for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Nutrition's Impact on Testosterone: Deficiencies and Dietary Solutions for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Respiratory Health's Impact on Testosterone Levels in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Testosterone's Role and Managing Low Levels in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Low Testosterone Linked to Anemia Risk in American Men: Insights and Management [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Low Testosterone Linked to Autoimmune Diseases in American Men: Insights and Management [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Liver Health Crucial for Testosterone Balance in American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Gut Health and Testosterone: Optimizing Hormonal Balance in American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Low Testosterone Linked to Increased Kidney Disease Risk in American Men [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Dental Health's Role in Managing Low Testosterone in American Males [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Low Testosterone Linked to Neurological Risks in American Men: Implications and Interventions [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Low Testosterone Linked to Increased Eye Disorder Risk in American Men [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Low Testosterone's Impact on Musculoskeletal Health in American Men: Risks and Interventions [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- ENT Health's Crucial Role in Maintaining Testosterone Levels in American Men [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Reproductive Health's Impact on Testosterone Levels in American Males [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Low Testosterone Levels Increase Infectious Disease Risk in American Men: Emerging Evidence [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Low Testosterone and Hematological Risks in American Men: Screening and Treatment Insights [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Managing Low Testosterone: Endocrine Health and Holistic Approaches for American Males [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Immunological Health's Impact on Testosterone Levels in American Males: A Holistic Approach [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Cancer's Impact on Testosterone Levels in American Men: Challenges and Management [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Low Testosterone Linked to Increased Psychiatric Disorders in American Men: Implications and Treatments [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Low Testosterone and Urological Health: Risks, Links, and Management Strategies for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Testosterone Levels and Wound Healing in American Males: A Bidirectional Impact Study [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Low Testosterone Linked to Increased Vascular Disorder Risk in American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Rheumatological Disorders and Low Testosterone: Insights and Management for American Males [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Low Testosterone's Impact on Surgical Risks in American Men: A Comprehensive Review [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Trauma's Impact on Testosterone Levels in American Males: Mechanisms and Management [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Low Testosterone and Genetic Disorders: Risks and Management in American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Developmental Health Impacts on Testosterone Levels in American Males: A Comprehensive Analysis [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Low Testosterone in American Men Linked to Increased Congenital Disorder Risk in Offspring [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Low Testosterone in American Men Linked to Pediatric Disorders in Offspring [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Occupational Health Impacts on Testosterone Levels in American Males: A Comprehensive Analysis [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Low Testosterone Linked to Increased Allergic Reactions in American Men: Emerging Evidence [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Anesthetic Health and Its Impact on Low Testosterone in American Males [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Low Testosterone Risks in Aging American Men: Health Impacts and Management Strategies [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Neonatal Health's Long-term Impact on Testosterone Levels in American Males [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Prenatal Health's Impact on Adult Male Testosterone Levels and Management Strategies [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Managing Low Testosterone: Diagnosis, Treatment Options, and Lifestyle Strategies [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
- Low Testosterone Linked to Higher Type 2 Diabetes Risk in American Males [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
Word Count: 560