Video Link: https://vimeo.com/291650795
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
To provide the best possible HRT Care, available treatments must be prescribed with the latest in medical research in mind.
Earlier this month, the American Urological Association released updated guidelines regarding the diagnosis and treatment of Low-T and the ongoing assessment of men taking Prescription Testosterone.
 While Testosterone Deficiency is a widespread medical issue, it is essential to make sure that Testosterone is only prescribed to those that have a demonstrative need for Hypogonadism Treatment.
While Testosterone Deficiency is a widespread medical issue, it is essential to make sure that Testosterone is only prescribed to those that have a demonstrative need for Hypogonadism Treatment.
It is best practices for patients taking Testosterone to undergo periodic evaluation. Still, this part of the process is frequently overlooked, which may be detrimental to the long-term care of the patient.
American Urological Association Guidelines have been released as the result of over 500 articles published over the last 40 years. A primary design goal of these guidelines was to assess the medical support of various claims regarding Bio-Identical Testosterone Therapy.
What is the Minimum Threshold for Testosterone Deficiency Diagnosis?
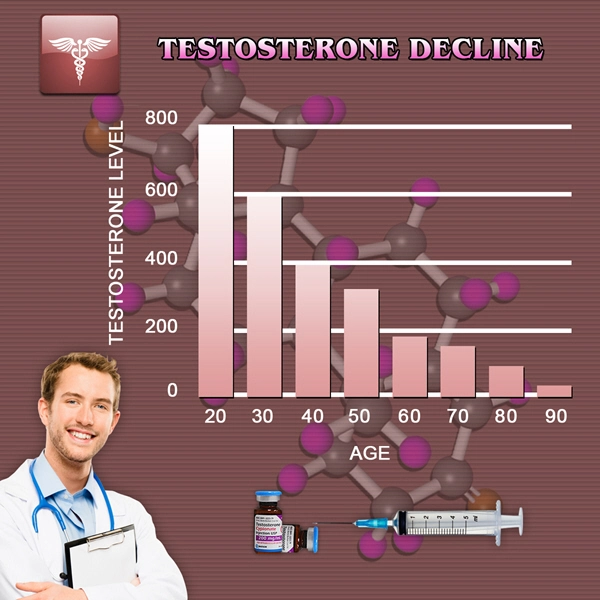
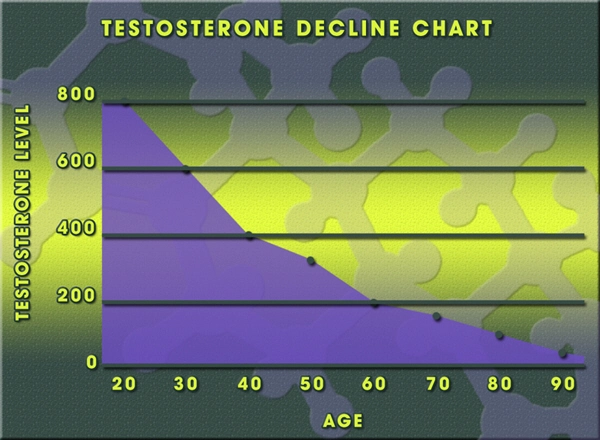
 While the normal range for Testosterone is considered to be between 270-1,070 ng/dl, the American Urological Association suggests that only patients below 300 ng/dL be regarded as candidates for Low-T Treatment, while leaving some room for discretion by the prescribing Testosterone Doctor.
While the normal range for Testosterone is considered to be between 270-1,070 ng/dl, the American Urological Association suggests that only patients below 300 ng/dL be regarded as candidates for Low-T Treatment, while leaving some room for discretion by the prescribing Testosterone Doctor.
Ideally, Total Testosterone Concentrations should be measured at least twice before reaching a Low-T Diagnosis.
Also, Low Testosterone Levels alone should not be considered sufficient evidence of Testosterone Deficiency — the patient should also show symptoms of the Hormonal Condition.
Who Should Undergo Low-T Evaluation?
Testosterone Deficiency is not only the result of aging, but a variety of other lifestyle factors, medical events, and health history.
The American Urological Associated suggests further investigation of Low Testosterone Levels for patients under the following circumstances:
- Low Libido
- Sexual Insufficiency
- Diabetes
- Loss of Bone Mineral Density
- Chronic Use of Corticosteroids or Narcotics
- Prior Radiation or Chemotherapy
- HIV/AIDS
- Pituitary Abnormalities
- Anemia
What Tests Should be Performed in Conjunction With Low-T Analysis?
 When monitoring for Testosterone Deficiency, it's essential to investigate other underlying issues that can help reveal the source of diminishing Testosterone Levels.
When monitoring for Testosterone Deficiency, it's essential to investigate other underlying issues that can help reveal the source of diminishing Testosterone Levels.
In particular, it is essential to measure Luteinizing Hormone Levels because this secretagogue is a crucial Testosterone Precursor. HRT Doctors should also monitor Prolactin Levels along with Luteinizing Hormone.
If Prolactin Levels are elevated, this is a sign that Low-T is likely the result of another underlying Endocrine Disorder.
For safety reasons, patients should have Hemoglobin, and Red Blood Cell Count monitored, because Testosterone Injections, Creams, and Patches can lead to Polycythemia (elevated RBC Concentration).
The American Urological Association recommends against the prescription of Alkylated Oral Testosterone because of the risk of side-effects associated with liver toxicity.
What Should Doctors Let Their Patients Know Before They Suggest Low-T Therapy as an Option?
Potential Testosterone Therapy Patients must be fully informed  about the benefits and drawbacks of Bio-Identical Testosterone.
about the benefits and drawbacks of Bio-Identical Testosterone.
It's also important to differentiate between conclusively proven benefits and potential benefits that have not been sufficiently proven at this time.
The American Urological Association recommends that Hormone Doctors and Endocrinologists tell their patients about the correlation between heart disease and Low-T.
Men should also be informed that Bio-Identical Testosterone can provide relief from depression and anemia, improve body composition, enhance sexual desire and function, and increase Bone Mineral Density.
On the other hand, they should also be adequately informed that there is insufficient evidence to prove that Testosterone improves Cholesterol Levels, increases energy, diminishes fatigue, enhances cognition, or reduces diabetic issues.
Shortly, it is very likely that these benefits will manifest more clearly, but for now, the evidence isn't available in an appropriate volume.
What is the Ultimate Therapeutic Goal of Testosterone Therapy?
The American Urological Association recommends that Testosterone Levels be increased to the middle of the normal range for optimal treatment with the minimized risk of side effects.
By bringing Testosterone Levels up to this threshold, it's possible to provide patients with significant benefits.
To ensure that the treatment is providing the desired results and to monitor progress, Testosterone Levels should be reassessed either 1-2 times per year to make sure that the patient is maintaining ideal Serum Testosterone (not too high/too low).
If, after 3-6 months of treatment, the patient doesn't see noticeable results, doctors should suggest that the patient quit taking Testosterone.
Men Looking to Conceive Should Not Take Testosterone — Other HRT Options Available
Men that are concerned with maintaining fertility should not be given Testosterone Therapy. Taking Testosterone for an extended period significantly reduces fertility.
Bio-Identical Testosterone Treatments can vastly diminish the concentrations of essential Testosterone Precursors necessary for optimal fertility, leading to temporary practical infertility. For these patients, Selective Estrogen Receptor Modulators, HCG Injections, and Aromatase Inhibitors can all enhance Testosterone Levels without the use of an Exogenous Testosterone Supply.
Who Should Avoid Testosterone?
At this time, certain men should avoid Testosterone until further evidence proves its safety in exceptional cases. For example, patients at high risk of Prostate Cancer should not take Testosterone.
A Prostate-Specific Antigen (PSA) Test should be conducted before Testosterone Therapy Treatment. Also, there is insufficient evidence regarding the effect of Testosterone Therapy on patients that have experienced traumatic cardiovascular events in the past.
Talk to your General Practitioner or Hormone Specialist for more details.
Reference
Evaluation and Management of Testosterone Deficiency
Contact Us Today For A Free Consultation

- Washington D.C. Testosterone Clinics for Low-T and Hormone Therapy [Last Updated On: October 1st, 2024] [Originally Added On: July 16th, 2018]
- Columbia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 2nd, 2024] [Originally Added On: November 11th, 2018]
- Charleston Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 14th, 2024] [Originally Added On: November 11th, 2018]
- Providence Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 24th, 2024] [Originally Added On: November 11th, 2018]
- Pittsburgh Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 7th, 2024] [Originally Added On: November 11th, 2018]
- Philadelphia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 15th, 2024] [Originally Added On: November 11th, 2018]
- Erie Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 22nd, 2024] [Originally Added On: November 11th, 2018]
- Allentown Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 10th, 2024] [Originally Added On: November 11th, 2018]
- Salem Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 6th, 2024] [Originally Added On: November 11th, 2018]
- Portland Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 11th, 2024] [Originally Added On: November 11th, 2018]
- Gresham Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 13th, 2024] [Originally Added On: November 11th, 2018]
- Eugene Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 19th, 2024] [Originally Added On: November 11th, 2018]
- Tulsa Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 13th, 2024] [Originally Added On: November 11th, 2018]
- Oklahoma City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 18th, 2024] [Originally Added On: November 11th, 2018]
- Norman Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 20th, 2024] [Originally Added On: November 11th, 2018]
- Toledo Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 21st, 2024] [Originally Added On: November 11th, 2018]
- Dayton Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 4th, 2024] [Originally Added On: November 11th, 2018]
- Columbus Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 24th, 2024] [Originally Added On: November 11th, 2018]
- Cleveland Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 12th, 2024] [Originally Added On: November 11th, 2018]
- Cincinnati Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 5th, 2024] [Originally Added On: November 11th, 2018]
- Akron Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 1st, 2024] [Originally Added On: November 11th, 2018]
- Bismarck Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 17th, 2024] [Originally Added On: November 11th, 2018]
- Winston-Salem Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 15th, 2024] [Originally Added On: November 11th, 2018]
- Wilmington Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 29th, 2024] [Originally Added On: November 11th, 2018]
- Raleigh Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 29th, 2024] [Originally Added On: November 11th, 2018]
- High Point Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 10th, 2024] [Originally Added On: November 11th, 2018]
- Greensboro Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 30th, 2024] [Originally Added On: November 11th, 2018]
- Fayetteville Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 19th, 2024] [Originally Added On: November 11th, 2018]
- Durham Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 24th, 2024] [Originally Added On: November 11th, 2018]
- Charlotte Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 7th, 2024] [Originally Added On: November 11th, 2018]
- Cary Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 16th, 2024] [Originally Added On: November 11th, 2018]
- Yonkers Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 7th, 2024] [Originally Added On: November 11th, 2018]
- Syracuse Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 10th, 2024] [Originally Added On: November 11th, 2018]
- Rochester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 16th, 2024] [Originally Added On: November 11th, 2018]
- Buffalo Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 5th, 2024] [Originally Added On: November 11th, 2018]
- Albuquerque Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 28th, 2024] [Originally Added On: November 11th, 2018]
- Paterson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 14th, 2024] [Originally Added On: November 11th, 2018]
- Newark Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 9th, 2024] [Originally Added On: November 11th, 2018]
- Jersey City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 19th, 2024] [Originally Added On: November 11th, 2018]
- Elizabeth Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 15th, 2024] [Originally Added On: November 11th, 2018]
- Manchester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 27th, 2024] [Originally Added On: November 11th, 2018]
- Reno Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 26th, 2024] [Originally Added On: November 11th, 2018]
- North Las Vegas Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 2nd, 2024] [Originally Added On: November 11th, 2018]
- Las Vegas Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 7th, 2024] [Originally Added On: November 11th, 2018]
- Henderson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 17th, 2024] [Originally Added On: November 11th, 2018]
- Omaha Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 17th, 2024] [Originally Added On: November 11th, 2018]
- Lincoln Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 30th, 2024] [Originally Added On: November 11th, 2018]
- Billings Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: June 8th, 2024] [Originally Added On: November 11th, 2018]
- St Louis Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: July 1st, 2024] [Originally Added On: November 11th, 2018]
- Springfield Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 1st, 2024] [Originally Added On: November 11th, 2018]
- Kansas City Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 4th, 2024] [Originally Added On: November 11th, 2018]
- Independence Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 12th, 2024] [Originally Added On: November 11th, 2018]
- Columbia Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 14th, 2024] [Originally Added On: November 11th, 2018]
- Jackson Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 20th, 2024] [Originally Added On: November 11th, 2018]
- St Paul Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 12th, 2024] [Originally Added On: November 11th, 2018]
- Rochester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 3rd, 2024] [Originally Added On: November 11th, 2018]
- Minneapolis Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: November 6th, 2024] [Originally Added On: November 11th, 2018]
- Warren Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 10th, 2024] [Originally Added On: November 11th, 2018]
- Sterling Heights Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 13th, 2024] [Originally Added On: November 11th, 2018]
- Lansing Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 25th, 2024] [Originally Added On: November 11th, 2018]
- Grand Rapids Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: April 19th, 2024] [Originally Added On: November 11th, 2018]
- Flint Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 20th, 2024] [Originally Added On: November 11th, 2018]
- Detroit Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 23rd, 2024] [Originally Added On: November 11th, 2018]
- Ann Arbor Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 3rd, 2024] [Originally Added On: November 11th, 2018]
- Worcester Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 28th, 2024] [Originally Added On: November 11th, 2018]
- Springfield Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 15th, 2024] [Originally Added On: November 11th, 2018]
- Lowell Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: January 25th, 2024] [Originally Added On: November 11th, 2018]
- Cambridge Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 6th, 2024] [Originally Added On: November 11th, 2018]
- Boston Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: August 16th, 2024] [Originally Added On: November 11th, 2018]
- Baltimore Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 7th, 2024] [Originally Added On: November 11th, 2018]
- Augusta Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: May 21st, 2024] [Originally Added On: November 11th, 2018]
- Shreveport Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 2nd, 2024] [Originally Added On: November 11th, 2018]
- New Orleans Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 16th, 2024] [Originally Added On: November 11th, 2018]
- Lafayette Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: September 24th, 2024] [Originally Added On: November 11th, 2018]
- Baton Rouge Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 2nd, 2024] [Originally Added On: November 11th, 2018]
- Louisville Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 23rd, 2024] [Originally Added On: November 11th, 2018]
- Lexington Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: October 11th, 2024] [Originally Added On: November 11th, 2018]
- Wichita Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: March 26th, 2024] [Originally Added On: November 11th, 2018]
- Topeka Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 28th, 2024] [Originally Added On: November 11th, 2018]
- Overland Park Testosterone Clinics for Low-T and Comprehensive Hormone Therapy [Last Updated On: February 20th, 2024] [Originally Added On: November 11th, 2018]
Word Count: 886