Testosterone Replacement Therapy DOES NOT Increase Heart Attack Risk
Recently, the mainstream media began sounding dire warnings about Testosterone Replacement Therapy (TRT).
Video Link: https://vimeo.com/291313917
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
Video Link: https://vimeo.com/291314001
Video Download: Click Here To Download Video
Video Stream: Click Here To Stream Video
A recent study was published by the non-profit journal, PLOS One, claiming that in the initial three months of TRT, men were more likely to experience a heart attack if they have previously experienced the cardiovascular disease.
However, when looked at unemotionally and in detail, the study appears to have overlooked several key factors.
This is just one of a barrage of studies that have employed questionable methodologies but used shock value and fear tactics that resulted in hysterical headlines across television, print, and the web.
 If that weren't enough, a similar study was released last year in the Journal of the American Medical Association (JAMA), which also concluded that Testosterone injections and creams increase the risk of a heart attack.
If that weren't enough, a similar study was released last year in the Journal of the American Medical Association (JAMA), which also concluded that Testosterone injections and creams increase the risk of a heart attack.
That study also had numerous issues that led to faulty conclusions.
Let's take a look at them.
The Important Relationship of Estrogen and Red Blood Cell Counts to Testosterone
Both studies mentioned above contained a glaring error: neither study measured Testosterone levels before and after Testosterone treatment.
Also, there was yet another massive problem with the methodologies of both of these studies: they failed to perform necessary screening tests before treatment started that would have likely disqualified some high-risk patients from receiving the therapy, including Estrogen Testing and the Complete Blood Count.
This lack of screening was inexcusable.
These two tests are crucial because elevated estrogen levels and red blood cell counts have been previously associated with an increased risk of complication when administering TRT.
The three variables of Endogenous Testosterone Production, Estrogen Production, and Red Blood Cell Count are all tests that are required to determine both whether a patient qualifies for therapy or needs to cease treatment.
Therefore, since these crucial tests were conveniently forgotten, many mistakenly believe patients should be informed that Testosterone Replacement Therapy increases the risk of heart disease and heart attack as a direct result of treatment.
This is one time when doctors should be aware of TRT's realities.
Our physicians are undoubtedly dedicated to their patient's well-being.
However, they can't be on top of every new treatment.
This is why it's crucial to increase physicians’ awareness regarding particular issues that can raise the potential risks of Testosterone Replacement.
High Red Blood Cell Counts Easy to Treat
Medical professionals must monitor all three of these variables before and during TRT to minimize the health risk to the patient.
Even if these tests indicate that problems are arising from TRT, these problems have solutions.
indicate that problems are arising from TRT, these problems have solutions.
For example, suppose the patient has an elevated RBC count after several months of therapy. In that case, the physician can adjust the Testosterone Dosage or only make sure the patient donates blood to decrease his RBC count, substantially reducing the risks of heart attack, stroke, and clotting.
Medications Available to Control Estrogen Safely
High Estrogen also increases stroke and heart attack risk, but it can be monitored and treated with an elevated RBC count.
If tests show that the patient is suffering from high Estrogen levels, powerful and effective medications can control Estrogen Levels, reducing them to normal.
The sad fact is this: these studies DID NOT perform due diligence to protect their patients from the well-documented and easily preventable risks associated with TRT, and they got wrong, insufficient data as a result.
Viagra Used by Control Patients Significantly Distorts Results
Still another problem with this study is this: several men were taking PDE5 inhibitors, and this group was compared to other patients WHO WERE NOT taking PDE5 medication.
It seems evident that the study's authors would have disclosed this in the name of scientific objectivity.
But this critical fact was ignored and not mentioned at all...not one word.
Researchers discovered that patients taking these medications (Viagra and Cialis), were less likely to experience heart complications during treatment.
The authors included PDE5 inhibitors in an attempt to make sure all patients were able to perform sexually.
They used PDE5 drugs to control for the improved libido associated with increased Testosterone.
 They ignored that PDE5 inhibitors not only affect sexual function in males but can also affect cardiovascular health in several beneficial ways.
They ignored that PDE5 inhibitors not only affect sexual function in males but can also affect cardiovascular health in several beneficial ways.
Two forms of PDE5 Inhibitors have been FDA-approved for the treatment of hypertension because these medications can reduce blood pressure by relaxing blood vessels.
The Journal of Cardiovascular Pharmacology and Therapeutics recently released a study that provides compelling evidence that PDE5 Inhibitors are useful as heart drugs for people suffering from coronary artery disease.
The study also points out that these drugs can improve heart failure patients' health outcomes.
The potential cardiovascular benefits of PDE5 Inhibitors make these drugs a safe method of controlling potential heart risks of TRT since men taking PDE5 drugs will have healthier hearts on average than men who don't take them.
By ignoring this fundamental fact, the study makes TRT appear more dangerous than it is.
Latest Research Indicates Testosterone Replacement Therapy is Safe
Although this PLOS One study is receiving tons of media coverage, it contradicts twenty years of research showing that testosterone patches, injections, and creams can improve heart health by increasing muscle mass and reducing body fat while balancing blood sugar and cholesterol.
The combined outcomes of earlier research like the PLOS One study have left doctors without concrete tips on treating males for low testosterone (“Low-T”), with the FDA advising against over-prescription due to a high danger of coronary heart assault and stroke.
However, the Times are Changing
The Journal of the American Heart Association recently released a research survey that further reduces the credibility of the PLOS One article.
In this review, over one hundred studies were analyzed, searching for evidence of how TRT impacts patients' cardiovascular health.
Their conclusion?
Testosterone deficiency is undeniably linked to severe mortality risks, including increased incidence of diabetes and obesity, an elevated risk of heart attack, stroke, and other dangerous cardiovascular conditions such as atherosclerosis.
Researchers also discovered that the more severe the testosterone deficiency, the more dangerous the symptoms manifested themselves.
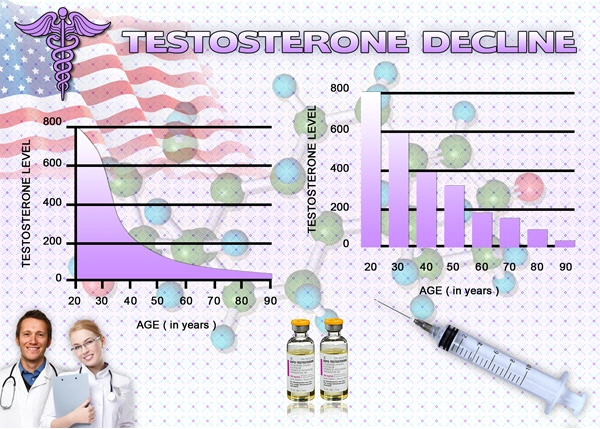
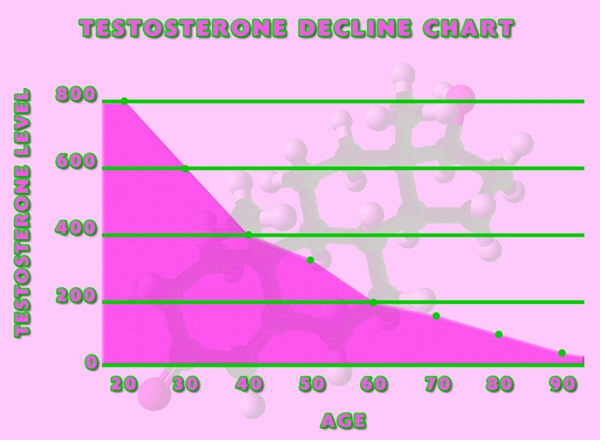
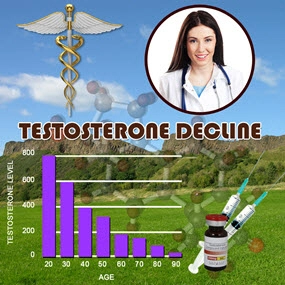
Testosterone is a hormone that acts as a "fountain of youth" in some ways for men.
The chemical peaks in male bodies during their teen years and declines as men grow older.
men grow older.
Symptoms of this loss can include reduced sexual desire, sleeplessness, increased body fat, and hair loss.
This hormone can be replaced through injections, patches, or a topical gel.
Despite this, few studies have been conducted on the safety of supplementing the male sex hormone.
Low testosterone is becoming a more significant concern in recent years as people become more aware of the condition.
Some advertisements for prescription drugs encourage men feeling lethargic or losing interest in sex to ask their doctors about the hormone.
However, this does not always drive changes in men as they age.
"Sometimes it is testosterone, sometimes it is the thyroid, and sometimes it's something unrelated to hormones," according to Dr. Spyros Mezitis, a physician experienced in treating Low-T.
Further studies will examine testosterone's role in mitigating the risks of heart attacks and strokes.
Possible side effects in patients will also be reviewed to determine if the risks of TRT are manageable.
Earlier studies have suggested that such treatments could be tied to sleep apnea (rough breathing), the increased growth rate of prostate cancer, and blood clots.
A Veterans Administration Study Adds More Fuel to the Fire
A Veterans Administration study of more than 83,000 patients determined that men with low testosterone levels returned to normal had a lower risk of heart attack, stroke, or death than men who did not receive testosterone.
 The study also found that men treated but didn't regain healthy levels did not experience the same benefits as those whose levels reached an average range.
The study also found that men treated but didn't regain healthy levels did not experience the same benefits as those whose levels reached an average range.
The study was published online in the European Heart Journal on Aug. 6, 2015.
The conclusions might lead the way to a sea-change concerning testosterone therapy's benefits and risks, particularly for the heart.
Previous studies have produced mixed results, although differing patient populations and the research methods used might explain part of that.
For example, the new VA study excluded men with a history of heart attacks or strokes but did include those with existing heart disease.
A much-cited VA database study published in the Journal of the American Medical Association in 2013 focused on men with coronary artery disease; about 20 percent of the total study group of around 8,700 men had suffered a previous heart attack.
To date, the medical community lacks conclusions from a final clinical trial that might provide definitive recommendations.
Meanwhile, the Food and Drug Administration (FDA) issued guidance in 2015 warning physicians about overusing testosterone therapy and referring to a possible increased risk of heart attack and stroke.
A Potential Game-Changer
The new VA study is a potential game-changer due to its large size and relatively extended follow-up period.
Dr. Rajat Barua, the study's corresponding author, says the research is also crucial because of its finding that administering the correct dose is critical: Treating "low-T" but not restoring levels to standard doesn't appear to deliver many benefits, at least concerning cardiovascular risk.
Testosterone isn't prescribed to improve heart health, but it is a factor considered in many cases.
"It is the first study to demonstrate that significant benefit is observed only if the dose is adequate to normalize the total testosterone levels," Barua and his  coauthors wrote.
coauthors wrote.
"Patients who failed to achieve the therapeutic range after testosterone replacement therapy did not see a reduction in [heart attack] or stroke and had significantly less benefit on mortality."
Barua is affiliated with the Kansas City (Mo.) VA Medical Center. He's also an assistant professor of medicine at the University of Kansas.
The study team reviewed national data on more than 83,000 men with verified low testosterone, all age 50 or above, who received treatment in the VA between 1999 and 2014.
The researchers divided the men into three clinical groups: those who had their total testosterone levels returned to normal (Group 1), those who were treated but did not obtain healthy levels (Group 2), and those who were untreated and remained at low testosterone levels (Group 3).
Most importantly, all three groups were "propensity-matched" so the comparisons could be made between men with similar health profiles.
Unlike the earlier studies mentioned above, the researchers considered various factors that might affect cardiovascular and overall risk: age, body mass index, chronic diseases, LDL cholesterol levels, aspirin use, beta-blockers, and statins.
The average follow-up across the groups ranged from 4.6 to 6.2 years.
The most significant difference was between Group 1 (those treated and attained normal levels) and Group 3 (those whose low testosterone went untreated).
The treated men were 56 percent less likely to die during the follow-up period, 24 percent less likely to suffer a heart attack, and 36 percent less likely to have a stroke.
The differences between Group 1 and Group 2 (those treated but did not regain normal levels) were similar but less pronounced.
Groups 2 and 3 showed little difference, except for a slight benefit in survival for those treated.
Barua and colleagues say they cannot determine the exact reasons for testosterone's apparent advantages for the heart and overall survival.
"The mechanisms for these effects remain speculative," they write.
Possible explanations, they say, could involve body fat, insulin sensitivity, lipids, blood platelets, inflammation, or other biological pathways.
More research is required, they insist, to determine how testosterone affects the cardiovascular system.
 The authors also warn that "off-label" use remains problematic. Physicians should not only reach for the prescription pad because an elderly man is complaining of symptoms such as low energy and sex drive.
The authors also warn that "off-label" use remains problematic. Physicians should not only reach for the prescription pad because an elderly man is complaining of symptoms such as low energy and sex drive.
According to the FDA, "Testosterone products are FDA-approved only for use in men who lack or have low testosterone levels in conjunction with an associated medical condition.
Examples of these circumstances include failure of the testicles to produce testosterone because of reasons such as genetic problems or chemotherapy...none of the FDA-approved testosterone products are approved for use in men with low testosterone levels who lack an associated medical condition."
Further studies will examine testosterone's role in mitigating the risks of heart attacks and strokes.
Possible side effects in patients will also be reviewed to determine if the risks of TRT are manageable.
Earlier studies have suggested that such treatments could be tied to sleep apnea (rough breathing), the increased growth rate of prostate cancer, and blood clots.
The literature review offers near-incontrovertible evidence that Testosterone Replacement Therapy improves heart health by relaxing the coronary arteries and helping men with heart failure to engage in physical exercise.
Testosterone HRT has also been shown to reduce BMI and control blood sugar in patients who have diabetes, which also preserves heart health and reduces mortality risk.
Single studies are often inaccurate, and the PLOS One study seems to be in that category.
Remember this the next time you hear about a single study espousing the potential dangers of TRT.
Recent research suggests that's not the case, and it will take robust evidence to prove otherwise.
Reference
Study of 83,000 Veterans finds cardiovascular benefits to testosterone replacement
Contact Us Today For A Free Consultation

- Adverse Effects of Testosterone Therapy in Adult Men: A Systematic Review and Meta-Analysis [Last Updated On: July 2nd, 2024] [Originally Added On: June 4th, 2010]
- Low Testosterone Levels, Foods That Increase Testosterone Levels wwwSelf-Improvement-Bible.com [Last Updated On: November 12th, 2023] [Originally Added On: May 30th, 2011]
- Low Testosterone in Men: The Next Big Thing in Medicine! - Abraham Morgentaler, MD [Last Updated On: May 7th, 2023] [Originally Added On: June 3rd, 2011]
- How To Determine Testosterone Levels By Looking At Your Ring Finger [Last Updated On: December 7th, 2017] [Originally Added On: June 30th, 2011]
- Prolab Horny Goat Weed Testosterone Booster Supplement Review [Last Updated On: November 23rd, 2023] [Originally Added On: July 19th, 2011]
- The Healthy Skeptic: Products make testosterone claims [Last Updated On: August 13th, 2024] [Originally Added On: September 11th, 2011]
- How To Naturally Increase Testosterone [Last Updated On: November 21st, 2023] [Originally Added On: September 28th, 2011]
- Testosterone Production - Video [Last Updated On: November 25th, 2024] [Originally Added On: November 20th, 2011]
- Testosterone makes us less cooperative and more egocentric, study finds [Last Updated On: January 23rd, 2018] [Originally Added On: February 1st, 2012]
- Testosterone makes us less cooperative and more egocentric [Last Updated On: January 24th, 2018] [Originally Added On: February 1st, 2012]
- Too much testosterone makes for bad decisions, tests show [Last Updated On: April 30th, 2025] [Originally Added On: February 1st, 2012]
- Today in Research: Testosterone's Negative Effects; Diet Soda Death [Last Updated On: January 2nd, 2018] [Originally Added On: February 2nd, 2012]
- Testosterone drives ego, trips cooperation [Last Updated On: December 2nd, 2017] [Originally Added On: February 4th, 2012]
- FDA approves BioSante/Teva's testosterone gel [Last Updated On: April 28th, 2025] [Originally Added On: February 15th, 2012]
- 'Manly' Fingers Make For Strong Jawline in Young Boys [Last Updated On: December 1st, 2017] [Originally Added On: February 15th, 2012]
- Teva, BioSante Win U.S. Approval for Testosterone Therapy [Last Updated On: December 10th, 2017] [Originally Added On: February 15th, 2012]
- BioSante Gains on Approval of Testosterone Gel: Chicago Mover [Last Updated On: January 8th, 2018] [Originally Added On: February 16th, 2012]
- BioSante soars following drug approval from FDA [Last Updated On: December 26th, 2017] [Originally Added On: February 16th, 2012]
- Antibodies, Not Hard Bodies: The Real Reason Women Drool Over Brad Pitt [Last Updated On: December 24th, 2017] [Originally Added On: February 21st, 2012]
- Almark Publishing Releases Book From Mark Rosenberg, M.D. Revealing Natural Discoveries Associated With Low ... [Last Updated On: May 3rd, 2025] [Originally Added On: February 28th, 2012]
- Testosterone Replacement Clinic Comes to Kansas City with Potential to Help Thousands of Men [Last Updated On: May 2nd, 2025] [Originally Added On: March 1st, 2012]
- Study examines the relative roles of testosterone and its metabolite, dihydrotestosterone in men [Last Updated On: December 2nd, 2017] [Originally Added On: March 7th, 2012]
- The Role of 5{alpha}-Reductase Inhibition in Men Receiving Testosterone Replacement Therapy [Editorial] [Last Updated On: December 21st, 2017] [Originally Added On: March 7th, 2012]
- Effect of Testosterone Supplementation With and Without a Dual 5{alpha}-Reductase Inhibitor on Fat-Free Mass in Men ... [Last Updated On: January 3rd, 2018] [Originally Added On: March 7th, 2012]
- Why We Like Men Who Can Keep Their Cool [Last Updated On: December 30th, 2017] [Originally Added On: March 7th, 2012]
- Testosterone And Heart Health [Last Updated On: May 1st, 2025] [Originally Added On: March 10th, 2012]
- Your Life on Testosterone: Overly Sure of Yourself, Unwilling to Listen [Last Updated On: November 25th, 2018] [Originally Added On: March 15th, 2012]
- Mayo Clinic-TGen study role testosterone may play in triple negative breast cancer [Last Updated On: December 8th, 2017] [Originally Added On: March 23rd, 2012]
- A dose of testosterone might not cure what ails you [Last Updated On: January 23rd, 2018] [Originally Added On: March 25th, 2012]
- Green tea could aid athletes hide testosterone doping [Last Updated On: December 16th, 2017] [Originally Added On: March 25th, 2012]
- TGen Study Role Testosterone May Play in Triple Negative Breast Cancer [Last Updated On: December 6th, 2017] [Originally Added On: March 26th, 2012]
- Testosterone low, but responsive to competition, in Amazonian tribe [Last Updated On: January 23rd, 2018] [Originally Added On: March 28th, 2012]
- Competition-linked bursts of testosterone are fundamental aspect of human biology, study of Amazonian tribe suggests [Last Updated On: December 25th, 2017] [Originally Added On: March 28th, 2012]
- Playing football boosts testosterone levels by 30 percent! [Last Updated On: February 4th, 2024] [Originally Added On: March 28th, 2012]
- Testosterone low, but responsive to competition, in Amazonian tribe -- with slideshow [Last Updated On: December 9th, 2017] [Originally Added On: March 28th, 2012]
- The benefits of testosterone pellet therapy [Last Updated On: January 24th, 2018] [Originally Added On: March 29th, 2012]
- Low testosterone levels cause health woes [Last Updated On: November 25th, 2018] [Originally Added On: March 30th, 2012]
- Heart Failure Patients Getting Relief from Testosterone Supplements [Last Updated On: May 5th, 2025] [Originally Added On: April 21st, 2012]
- Study Finds Fatherhood Suppresses Testosterone [Last Updated On: May 4th, 2025] [Originally Added On: May 3rd, 2012]
- Low testosterone levels could raise diabetes risk for men [Last Updated On: January 26th, 2018] [Originally Added On: May 5th, 2012]
- Why low testosterone may increase your risk of diabetes [Last Updated On: November 25th, 2024] [Originally Added On: May 5th, 2012]
- Diabetes link to low testosterone [Last Updated On: November 25th, 2024] [Originally Added On: May 5th, 2012]
- Testosterone Linked to Weight Loss in Obese Men [Last Updated On: January 2nd, 2018] [Originally Added On: May 11th, 2012]
- Testosterone may help weight loss [Last Updated On: November 25th, 2024] [Originally Added On: May 11th, 2012]
- Testosterone-fuelled infantile males might be a product of Mom's behaviour [Last Updated On: December 25th, 2017] [Originally Added On: May 11th, 2012]
- Testosterone-fueled infantile males might be a product of Mom's behavior [Last Updated On: January 6th, 2018] [Originally Added On: May 11th, 2012]
- Testosterone supplements may help obese men lose weight [Last Updated On: January 5th, 2018] [Originally Added On: May 11th, 2012]
- Testosterone supplements 'can help men lose their middle-aged spread' [Last Updated On: November 25th, 2024] [Originally Added On: May 12th, 2012]
- Some doctors question safety of testosterone replacement therapy [Last Updated On: January 20th, 2018] [Originally Added On: May 15th, 2012]
- Health Canada Approves New Testosterone Topical Solution for Men [Last Updated On: May 15th, 2025] [Originally Added On: May 15th, 2012]
- Environment trumps genes in testosterone levels, study finds [Last Updated On: May 8th, 2025] [Originally Added On: May 15th, 2012]
- Global Testosterone Replacement Therapy (TRT) Industry [Last Updated On: May 7th, 2025] [Originally Added On: May 21st, 2012]
- Testosterone Fuels Boom, Swindler Sows Panic: Top Business Books [Last Updated On: January 13th, 2018] [Originally Added On: June 2nd, 2012]
- Increase in testosterone drug use [Last Updated On: April 12th, 2018] [Originally Added On: June 4th, 2012]
- Testosterone Promotes Agression Automatically [Last Updated On: January 29th, 2018] [Originally Added On: June 9th, 2012]
- Testosterone shown to help sexually frustrated women [Last Updated On: January 27th, 2018] [Originally Added On: June 9th, 2012]
- Research and Markets: Testosterone Replacement Therapy (TRT) - Global Strategic Business Report [Last Updated On: December 23rd, 2017] [Originally Added On: June 12th, 2012]
- Proposed testosterone testing of some female olympians challenged by Stanford scientists [Last Updated On: January 30th, 2018] [Originally Added On: June 14th, 2012]
- Testosterone Makes Bosses Into Jerks, Says Paul Zak [Last Updated On: January 8th, 2018] [Originally Added On: June 14th, 2012]
- Testosterone Therapy: A Misguided Approach to Erectile Dysfunction (ED) [Last Updated On: May 10th, 2025] [Originally Added On: June 20th, 2012]
- New drugs, new ways to target androgens in prostate cancer therapy [Last Updated On: January 8th, 2018] [Originally Added On: June 20th, 2012]
- Long-term testosterone treatment for men results in reduced weight and waist size [Last Updated On: January 19th, 2018] [Originally Added On: June 23rd, 2012]
- Declining testosterone levels in men not part of normal aging, study finds [Last Updated On: December 27th, 2017] [Originally Added On: June 23rd, 2012]
- Low testosterone not normal part of aging [Last Updated On: December 22nd, 2017] [Originally Added On: June 25th, 2012]
- Testosterone Does Not Necessarily Wane With Age [Last Updated On: December 6th, 2017] [Originally Added On: June 25th, 2012]
- Overweight men can boost low testosterone levels by losing weight [Last Updated On: December 10th, 2017] [Originally Added On: June 25th, 2012]
- Testosterone-replacement therapy improves symptoms of metabolic syndrome [Last Updated On: January 14th, 2018] [Originally Added On: June 26th, 2012]
- Testosterone therapy takes off pounds [Last Updated On: December 11th, 2017] [Originally Added On: June 26th, 2012]
- Weight loss may boost men's testosterone [Last Updated On: May 9th, 2025] [Originally Added On: June 27th, 2012]
- Low Testosterone? Study finds age may not be to blame [Last Updated On: May 12th, 2025] [Originally Added On: July 1st, 2012]
- Do you have low testosterone? [Last Updated On: December 15th, 2017] [Originally Added On: July 8th, 2012]
- Wall Streeters Buying Testosterone for an Edge [Last Updated On: May 11th, 2025] [Originally Added On: July 12th, 2012]
- Beefy Wall Street Traders rub on testosterone [Last Updated On: February 20th, 2024] [Originally Added On: July 12th, 2012]
- Tale of two runners exposes flawed Olympic thinking [Last Updated On: December 23rd, 2024] [Originally Added On: July 19th, 2012]
- Genetic markers for testosterone and estrogen level regulation identified [Last Updated On: January 6th, 2018] [Originally Added On: July 20th, 2012]
- BUSM researchers identify genetic markers for testosterone, estrogen level regulation [Last Updated On: December 18th, 2017] [Originally Added On: July 20th, 2012]
- DRS. OZ AND ROIZEN: How to reap the benefits of normal testosterone levels [Last Updated On: December 23rd, 2024] [Originally Added On: July 21st, 2012]
- How Testosterone Drives History [Last Updated On: December 24th, 2024] [Originally Added On: July 22nd, 2012]
- Testosterone replacement is "fountain of youth" for men [Last Updated On: January 3rd, 2018] [Originally Added On: July 27th, 2012]
- Pill for low testosterone in men heads for phase II clinical trials [Last Updated On: December 31st, 2017] [Originally Added On: August 2nd, 2012]
Word Count: 2182