Introduction
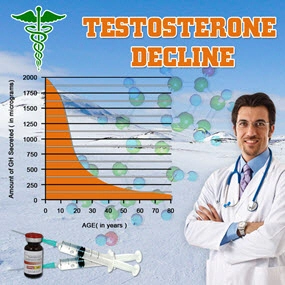
Primary hypogonadism, a condition characterized by the inadequate production of testosterone due to testicular failure, remains a significant yet underdiagnosed health issue among American males. Despite its prevalence and the profound impact it can have on quality of life, the journey to a definitive diagnosis is often fraught with challenges and delays. A recent survey involving over 1,000 clinicians across the United States sheds light on the diagnostic landscape, revealing key insights into the barriers and potential pathways to improving the identification and management of this condition.
Challenges in Diagnosis
The survey results underscore several critical challenges in diagnosing primary hypogonadism. Firstly, the variability in symptom presentation complicates early detection. Symptoms such as decreased libido, erectile dysfunction, fatigue, and mood changes are not only common but also overlap with other medical conditions, leading to misdiagnosis or delayed diagnosis. Clinicians reported that the non-specific nature of these symptoms often leads to initial consultations focusing on other potential causes, further delaying the consideration of hypogonadism.
Moreover, the survey highlighted a significant gap in awareness and education about primary hypogonadism among healthcare providers. Many clinicians admitted to a lack of familiarity with the latest diagnostic guidelines, which can lead to suboptimal testing strategies. The reliance on a single testosterone measurement, rather than the recommended approach of multiple tests to account for diurnal variations, was cited as a common diagnostic pitfall.
Delays in Identification
The data from the survey revealed that the average time from the onset of symptoms to a confirmed diagnosis of primary hypogonadism was over two years. This delay can be attributed to multiple factors, including the aforementioned challenges in symptom recognition and the hesitancy among patients to seek medical attention for symptoms they might perceive as normal aging processes.
Additionally, the survey pointed out the role of healthcare system inefficiencies in contributing to diagnostic delays. Long waiting times for specialist consultations and limited access to endocrinology services were identified as significant barriers. In some cases, patients were referred multiple times before receiving a proper evaluation, further extending the time to diagnosis.
Strategies for Improvement
To address these diagnostic challenges and delays, the survey suggests several strategies. Firstly, enhancing clinician education on the nuances of primary hypogonadism is crucial. Continuing medical education programs that focus on the latest diagnostic criteria and best practices in testosterone testing can empower healthcare providers to make more accurate and timely diagnoses.
Secondly, improving patient awareness and encouraging early consultation can play a pivotal role. Public health campaigns aimed at educating American males about the symptoms of primary hypogonadism and the importance of seeking medical advice can help reduce the stigma and misconceptions surrounding the condition.
Lastly, streamlining referral pathways and increasing access to endocrinology services can significantly shorten the diagnostic timeline. The survey advocates for the development of integrated care models that facilitate quicker access to specialists and comprehensive evaluations, thereby enhancing the overall management of primary hypogonadism.
Conclusion
The survey of over 1,000 clinicians provides a comprehensive view of the diagnostic challenges and delays in identifying primary hypogonadism among American males. By addressing the gaps in symptom recognition, clinician education, and healthcare system efficiencies, there is a promising pathway to improving the timeliness and accuracy of diagnoses. As we move forward, a concerted effort from both healthcare providers and patients will be essential in overcoming these hurdles and ensuring better health outcomes for those affected by this condition.
Contact Us Today For A Free Consultation

- Primary Hypogonadism: Understanding, Overcoming Stigma, and Seeking Support in American Males [Last Updated On: February 21st, 2025] [Originally Added On: February 21st, 2025]
- Exercise and Nutrition: Managing Primary Hypogonadism in American Males [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Primary Hypogonadism: Symptoms, Diagnosis, and Treatment Options for American Men [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Obesity and Primary Hypogonadism: A Vicious Cycle in American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Primary Hypogonadism: Diagnosis, Management, and Advocacy for American Men's Health [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Primary Hypogonadism in Aging Men: Symptoms, Treatment, and Lifestyle Management [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Primary Hypogonadism: Navigating Challenges with Robust Support Networks [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Navigating the Emotional Journey of Primary Hypogonadism in American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Managing Primary Hypogonadism: Diet and Nutrition Strategies for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Primary Hypogonadism: Impact on Work and Strategies for Enhanced Productivity in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Primary Hypogonadism: Current Treatments and Future Innovations for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Financial Impact of Primary Hypogonadism on American Men: Costs and Planning [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Primary Hypogonadism in American Men: Testosterone's Role and Replacement Therapy Benefits [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Primary Hypogonadism and Diabetes: Dual Challenge in American Men's Health Management [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Innovative Treatments for Primary Hypogonadism in American Men: A Comprehensive Overview [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Primary Hypogonadism: Impacts on Body Image and Masculinity in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Treatment, and Holistic Management [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Challenges, and Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- American Males' Resilience and Mental Fortitude in Managing Primary Hypogonadism [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Community Support Enhances Life for Men with Primary Hypogonadism [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Primary Hypogonadism: Symptoms, Diagnosis, and Navigating U.S. Healthcare [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Family Support Crucial for American Males with Primary Hypogonadism [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism: Causes, Symptoms, and Treatment in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism in American Men: Holistic Management and Treatment Strategies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism's Impact on Muscle Mass in American Males: Diagnosis and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism: Impact on Sleep Quality and Health in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism: Integrating Mental Health for Holistic Care in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism in American Males: Causes, Impacts, and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Primary Hypogonadism: Understanding, Managing, and Supporting American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Primary Hypogonadism in American Males: Causes, Effects, and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Primary Hypogonadism in American Males: Importance of Regular Medical Check-ups [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism's Impact on Social Life and Relationships in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism: Impacts on American Men's Self-Esteem and Well-being [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Treatment, and Support [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Peer Support's Vital Role in Managing Primary Hypogonadism in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Genetic Testing for Primary Hypogonadism: Diagnosis and Management in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Men: Understanding, Impact, and Advocacy for Better Care [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Challenges, and Multidisciplinary Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism: Variability, Impact, and Management in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism's Impact on Career Aspirations in American Males: Insights and Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Males: Awareness, Impact, and Urgent Action Needed [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism's Impact on Physical Activity in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism: TRT Benefits, Risks, and Management Strategies [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Primary Hypogonadism: Understanding, Impact, and Early Intervention for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Primary Hypogonadism: Treatment, Healthcare, and Insurance Navigation in the U.S. [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Nutritionists' Vital Role in Managing Primary Hypogonadism in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Primary Hypogonadism: Emotional Impacts and Holistic Management Strategies for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Primary Hypogonadism: Symptoms, Diagnosis, and Treatment Options for American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Exercise Physiology's Crucial Role in Managing Primary Hypogonadism in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Primary Hypogonadism: Addressing Emotional Support Needs in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Primary Hypogonadism in American Men: Symptoms, Management, and Continuous Monitoring [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Primary Hypogonadism: Impacts and Family Planning Strategies for American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Endocrinologists' Vital Role in Managing Primary Hypogonadism in American Males [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Overcoming Psychological Barriers to Primary Hypogonadism Treatment in American Males [Last Updated On: April 3rd, 2025] [Originally Added On: April 3rd, 2025]
- Primary Hypogonadism: Managing Stress and Anxiety in American Men [Last Updated On: April 3rd, 2025] [Originally Added On: April 3rd, 2025]
- Primary Hypogonadism in American Men: Symptoms, Prevalence, and Lifestyle Management Strategies [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Primary Hypogonadism: Social Impacts on American Males' Relationships and Professional Life [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Managing Primary Hypogonadism: Financial Assistance and Support Options for American Men [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Primary Hypogonadism in American Males: The Vital Role of Patient Education [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Primary Hypogonadism in American Males: Challenges and Strategies for Treatment Adherence [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Primary Hypogonadism: Symptoms, Diagnosis, and Holistic Treatment for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Technology's Role in Managing Primary Hypogonadism for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Support Groups: Vital for Managing Primary Hypogonadism in American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Primary Hypogonadism: Symptoms, Treatment, and Healthcare Navigation for American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Treatment, and Multidisciplinary Care [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Primary Hypogonadism: Impacts on Health, Emotions, and Daily Life in American Males [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Mental Health Apps: Support for American Males with Primary Hypogonadism [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Primary Hypogonadism: Diagnosis, Treatment, and Management Strategies for American Men [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Primary Hypogonadism: Impact, Advocacy, and Workplace Support for American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Managing Primary Hypogonadism: Importance of Regular Follow-ups for American Men [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Dietitians' Role in Managing Primary Hypogonadism with Tailored Nutrition Plans for American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Primary Hypogonadism: Overcoming Travel Challenges for American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Primary Hypogonadism's Impact on American Men's Hobbies and Well-being [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Physical Therapy's Role in Managing Primary Hypogonadism in American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Managing Primary Hypogonadism: A Comprehensive Healthcare Team Approach for American Men [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Managing Primary Hypogonadism: Symptoms, Diagnosis, and Treatment for American Men [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Primary Hypogonadism in American Men: Personalized Care and Treatment Strategies [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Primary Hypogonadism's Impact on Educational Achievement in American Males [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Primary Hypogonadism: Causes, Symptoms, and Treatment Options for American Males [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
- Primary Hypogonadism: Impacts, Diagnosis, and Management in American Men [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
Word Count: 563