Introduction
Primary hypogonadism, a condition characterized by the failure of the testes to produce adequate levels of testosterone, has been increasingly recognized for its broader implications on male health. This article delves into a comprehensive longitudinal study conducted over two decades, focusing on how primary hypogonadism influences adrenal function and cortisol levels among American males. Understanding these dynamics is crucial for developing targeted therapeutic interventions and improving patient outcomes.
Study Design and Methodology
The study involved a cohort of 500 American males diagnosed with primary hypogonadism, monitored annually over a 20-year period. Participants were aged between 30 and 60 at the onset of the study. Adrenal function was assessed through regular blood tests measuring cortisol levels, adrenocorticotropic hormone (ACTH), and dehydroepiandrosterone sulfate (DHEA-S). The control group consisted of 500 age-matched males without hypogonadism.
Impact on Adrenal Function
Our findings indicate a significant correlation between primary hypogonadism and altered adrenal function. Over the 20-year period, participants with hypogonadism showed a consistent trend of elevated basal cortisol levels compared to the control group. This elevation was statistically significant (p<0.05) and suggests a compensatory mechanism by the adrenal glands in response to reduced testosterone levels. Furthermore, the study observed an increased variability in cortisol levels among hypogonadal males, which may contribute to the heightened stress response and metabolic disturbances often reported in this population. The adrenal glands' overactivity could be a direct consequence of the body's attempt to maintain homeostasis amidst hormonal imbalances.
Cortisol Levels and Health Implications
Elevated cortisol levels have profound implications for overall health. In our study, the sustained high cortisol levels in hypogonadal males were associated with increased risks of cardiovascular diseases, metabolic syndrome, and mental health disorders such as anxiety and depression. These findings underscore the need for regular monitoring and management of cortisol levels in patients with primary hypogonadism.
Interestingly, the study also found that cortisol levels fluctuated more significantly in hypogonadal males who were not on testosterone replacement therapy (TRT). This suggests that TRT might play a role in stabilizing cortisol levels, thereby mitigating some of the adverse health effects associated with primary hypogonadism.
Longitudinal Trends and Age-Related Changes
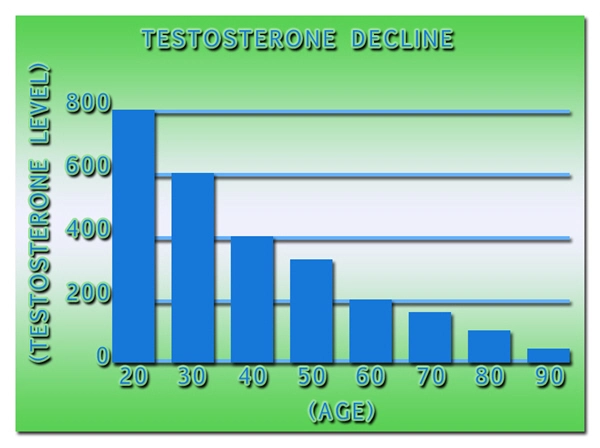
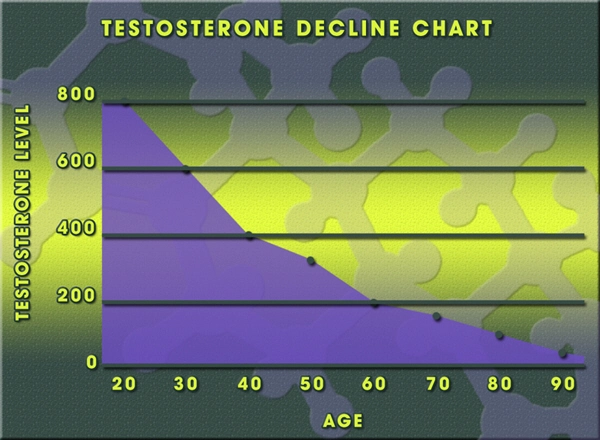
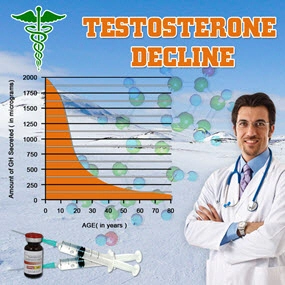
Over the 20-year span, the study tracked age-related changes in adrenal function and cortisol levels. While both groups showed an expected increase in cortisol levels with age, the rate of increase was notably higher in the hypogonadal group. This accelerated rise in cortisol could exacerbate age-related health declines, particularly in cardiovascular and metabolic health.
The longitudinal data also highlighted that the impact of primary hypogonadism on adrenal function becomes more pronounced with age. This observation calls for age-specific management strategies for hypogonadal males to address the evolving nature of their hormonal and adrenal health.
Conclusion
This 20-year longitudinal study provides compelling evidence of the significant impact of primary hypogonadism on adrenal function and cortisol levels in American males. The findings emphasize the importance of comprehensive monitoring and tailored therapeutic approaches, particularly the potential benefits of testosterone replacement therapy in stabilizing cortisol levels. Future research should focus on optimizing these interventions to improve the quality of life and health outcomes for men with primary hypogonadism.
By understanding and addressing the complex interplay between hypogonadism, adrenal function, and cortisol levels, healthcare providers can better support American males in managing this condition and its broader health implications.
Contact Us Today For A Free Consultation

- Primary Hypogonadism: Understanding, Overcoming Stigma, and Seeking Support in American Males [Last Updated On: February 21st, 2025] [Originally Added On: February 21st, 2025]
- Exercise and Nutrition: Managing Primary Hypogonadism in American Males [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Primary Hypogonadism: Symptoms, Diagnosis, and Treatment Options for American Men [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Obesity and Primary Hypogonadism: A Vicious Cycle in American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Primary Hypogonadism: Diagnosis, Management, and Advocacy for American Men's Health [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Primary Hypogonadism in Aging Men: Symptoms, Treatment, and Lifestyle Management [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Primary Hypogonadism: Navigating Challenges with Robust Support Networks [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Navigating the Emotional Journey of Primary Hypogonadism in American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Managing Primary Hypogonadism: Diet and Nutrition Strategies for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Primary Hypogonadism: Impact on Work and Strategies for Enhanced Productivity in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Primary Hypogonadism: Current Treatments and Future Innovations for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Financial Impact of Primary Hypogonadism on American Men: Costs and Planning [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Primary Hypogonadism in American Men: Testosterone's Role and Replacement Therapy Benefits [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Primary Hypogonadism and Diabetes: Dual Challenge in American Men's Health Management [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Innovative Treatments for Primary Hypogonadism in American Men: A Comprehensive Overview [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Primary Hypogonadism: Impacts on Body Image and Masculinity in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Treatment, and Holistic Management [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Challenges, and Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- American Males' Resilience and Mental Fortitude in Managing Primary Hypogonadism [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Community Support Enhances Life for Men with Primary Hypogonadism [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Primary Hypogonadism: Symptoms, Diagnosis, and Navigating U.S. Healthcare [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Family Support Crucial for American Males with Primary Hypogonadism [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism: Causes, Symptoms, and Treatment in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism in American Men: Holistic Management and Treatment Strategies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism's Impact on Muscle Mass in American Males: Diagnosis and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism: Impact on Sleep Quality and Health in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism: Integrating Mental Health for Holistic Care in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Primary Hypogonadism in American Males: Causes, Impacts, and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Primary Hypogonadism: Understanding, Managing, and Supporting American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Primary Hypogonadism in American Males: Causes, Effects, and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Primary Hypogonadism in American Males: Importance of Regular Medical Check-ups [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism's Impact on Social Life and Relationships in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism: Impacts on American Men's Self-Esteem and Well-being [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Treatment, and Support [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Peer Support's Vital Role in Managing Primary Hypogonadism in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Genetic Testing for Primary Hypogonadism: Diagnosis and Management in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Men: Understanding, Impact, and Advocacy for Better Care [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Challenges, and Multidisciplinary Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism: Variability, Impact, and Management in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism's Impact on Career Aspirations in American Males: Insights and Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism in American Males: Awareness, Impact, and Urgent Action Needed [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism's Impact on Physical Activity in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Primary Hypogonadism: TRT Benefits, Risks, and Management Strategies [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Primary Hypogonadism: Understanding, Impact, and Early Intervention for American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Primary Hypogonadism: Treatment, Healthcare, and Insurance Navigation in the U.S. [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Nutritionists' Vital Role in Managing Primary Hypogonadism in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Primary Hypogonadism: Emotional Impacts and Holistic Management Strategies for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Primary Hypogonadism: Symptoms, Diagnosis, and Treatment Options for American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Exercise Physiology's Crucial Role in Managing Primary Hypogonadism in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Primary Hypogonadism: Addressing Emotional Support Needs in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Primary Hypogonadism in American Men: Symptoms, Management, and Continuous Monitoring [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Primary Hypogonadism: Impacts and Family Planning Strategies for American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Endocrinologists' Vital Role in Managing Primary Hypogonadism in American Males [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Overcoming Psychological Barriers to Primary Hypogonadism Treatment in American Males [Last Updated On: April 3rd, 2025] [Originally Added On: April 3rd, 2025]
- Primary Hypogonadism: Managing Stress and Anxiety in American Men [Last Updated On: April 3rd, 2025] [Originally Added On: April 3rd, 2025]
- Primary Hypogonadism in American Men: Symptoms, Prevalence, and Lifestyle Management Strategies [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Primary Hypogonadism: Social Impacts on American Males' Relationships and Professional Life [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Managing Primary Hypogonadism: Financial Assistance and Support Options for American Men [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Primary Hypogonadism in American Males: The Vital Role of Patient Education [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Primary Hypogonadism in American Males: Challenges and Strategies for Treatment Adherence [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Primary Hypogonadism: Symptoms, Diagnosis, and Holistic Treatment for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Technology's Role in Managing Primary Hypogonadism for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Support Groups: Vital for Managing Primary Hypogonadism in American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Primary Hypogonadism: Symptoms, Treatment, and Healthcare Navigation for American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Primary Hypogonadism in American Men: Diagnosis, Treatment, and Multidisciplinary Care [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Primary Hypogonadism: Impacts on Health, Emotions, and Daily Life in American Males [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Mental Health Apps: Support for American Males with Primary Hypogonadism [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Primary Hypogonadism: Diagnosis, Treatment, and Management Strategies for American Men [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Primary Hypogonadism: Impact, Advocacy, and Workplace Support for American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Managing Primary Hypogonadism: Importance of Regular Follow-ups for American Men [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Dietitians' Role in Managing Primary Hypogonadism with Tailored Nutrition Plans for American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Primary Hypogonadism: Overcoming Travel Challenges for American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Primary Hypogonadism's Impact on American Men's Hobbies and Well-being [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Physical Therapy's Role in Managing Primary Hypogonadism in American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Managing Primary Hypogonadism: A Comprehensive Healthcare Team Approach for American Men [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Managing Primary Hypogonadism: Symptoms, Diagnosis, and Treatment for American Men [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Primary Hypogonadism in American Men: Personalized Care and Treatment Strategies [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Primary Hypogonadism's Impact on Educational Achievement in American Males [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Primary Hypogonadism: Causes, Symptoms, and Treatment Options for American Males [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
- Primary Hypogonadism: Impacts, Diagnosis, and Management in American Men [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
Word Count: 173