Introduction
Prostate health remains a significant concern for American men, with conditions such as benign prostatic hyperplasia (BPH) and prostate cancer affecting millions. Emerging research suggests a complex interplay between psychological stress and prostate health, mediated by psychoneuroendocrine pathways. This article delves into a prospective cohort study that explores how chronic stress influences prostate health in American men, offering insights into potential preventive strategies.
Study Design and Methodology
The study followed a cohort of 5,000 American men aged 40-70 over a five-year period. Participants were assessed for chronic stress levels using validated psychological scales, including the Perceived Stress Scale (PSS) and the Cohen-Hoberman Inventory of Physical Symptoms (CHIPS). Prostate health was monitored through annual PSA tests, digital rectal examinations, and self-reported symptoms of BPH. The study aimed to identify correlations between stress levels and the incidence and progression of prostate conditions.
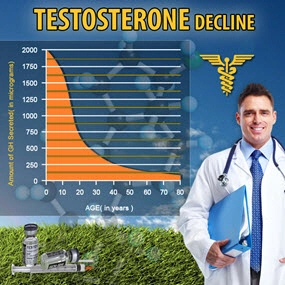
Psychoneuroendocrine Pathways: The Stress-Prostate Connection
Chronic stress triggers a cascade of physiological responses, primarily through the activation of the hypothalamic-pituitary-adrenal (HPA) axis. Elevated levels of cortisol, the primary stress hormone, can influence prostate cell proliferation and inflammation, potentially contributing to the development and progression of prostate diseases. The study found that men with higher stress scores exhibited significantly higher PSA levels and a greater incidence of BPH symptoms, suggesting a direct link between stress and prostate health.
Findings: Stress and Prostate Health Outcomes
The cohort study revealed a clear association between chronic stress and adverse prostate health outcomes. Men in the highest quartile of stress scores had a 30% increased risk of developing BPH and a 20% higher likelihood of experiencing a significant rise in PSA levels compared to those in the lowest quartile. These findings underscore the importance of addressing psychological stress as part of a comprehensive approach to prostate health management.
Implications for Clinical Practice
The study's results suggest that healthcare providers should consider screening for chronic stress in men at risk for prostate conditions. Implementing stress management interventions, such as cognitive-behavioral therapy (CBT) or mindfulness-based stress reduction (MBSR), could potentially mitigate the impact of stress on prostate health. Clinicians may also explore the use of biomarkers related to the HPA axis, such as cortisol levels, to better understand the psychoneuroendocrine pathways affecting prostate health.
Limitations and Future Research Directions
While the study provides valuable insights, it has limitations, including the reliance on self-reported stress measures and the potential influence of confounding factors such as diet and lifestyle. Future research should aim to elucidate the specific mechanisms by which stress affects prostate health, potentially through longitudinal studies with more objective stress assessments and genetic analyses. Additionally, randomized controlled trials evaluating the efficacy of stress reduction interventions on prostate health outcomes are warranted.
Conclusion
The prospective cohort study highlights the significant impact of chronic stress on prostate health in American men, mediated by psychoneuroendocrine pathways. These findings emphasize the need for a holistic approach to prostate health that includes stress management strategies. By addressing the psychological aspects of health, clinicians can potentially improve outcomes for men at risk of prostate conditions, ultimately enhancing their quality of life.
References
1. Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385-396.
2. Hoberman, H. M., & Cohen, S. (1983). The Cohen-Hoberman Inventory of Physical Symptoms (CHIPS): Factor structure and preliminary validation. Journal of Behavioral Medicine, 6(3), 257-271.
3. McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87(3), 873-904.
This article provides a comprehensive overview of the relationship between stress and prostate health in American men, offering valuable insights for both clinicians and patients.
Contact Us Today For A Free Consultation

- Prostate Health in Aging American Men: BPH, Cancer, and Lifestyle Management [Last Updated On: March 1st, 2025] [Originally Added On: March 1st, 2025]
- Prostate Health Essentials: Risks, Prevention, and Screening for American Men [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Understanding Benign Prostatic Hyperplasia: Symptoms, Diagnosis, and Management in American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Prostate Health and Cancer: The Crucial Role of Family History in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Exercise Regimen for Optimal Prostate Health in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Navigating Life After Prostate Cancer: Health, Well-being, and Survivorship Strategies [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Dietary Strategies for Enhancing Prostate Health in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Prostate Cancer Screening: Controversies, Guidelines, and Future Directions [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Prostate Cancer Treatments: Understanding and Managing Side Effects for American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Exercise as a Key to Prostate Health for American Males: Benefits and Recommendations [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Prostate Health and Heart Disease: Understanding the Connection and Risks for American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Prostate Cancer's Psychological Impact on American Men: Diagnosis to Recovery [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Prostate Health: Understanding Symptoms, Seeking Care, and Maintaining Wellness in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Prostate Cancer Stages and Grades: A Comprehensive Guide for American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Vitamin D's Role in Prostate Health: Insights and Recommendations for American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Environmental Factors and Prostate Health: Risks and Mitigation Strategies for American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Hydration's Vital Role in Prostate Health for American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Avoid These Foods for Better Prostate Health in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Palliative Care's Vital Role in Enhancing Prostate Cancer Management and Quality of Life [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Chemotherapy's Role in Managing Prostate Cancer: Efficacy and Quality of Life in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Active Surveillance: A Tailored Approach to Managing Low-Risk Prostate Cancer [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Prostate Cancer and Cryotherapy: Benefits, Risks, and Management for American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Prostate Cancer's Impact on Fertility: Treatments and Preservation Options [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Prostate Cancer and Radiation Therapy: Efficacy, Side Effects, and Future Advances [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- HIFU: A Minimally Invasive Hope for Prostate Cancer Treatment [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Prostate Cancer Treatment: Understanding Brachytherapy's Benefits and Procedure [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Sleep's Crucial Role in Prostate Health for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Prostate Cancer Support Groups: Emotional, Educational, and Practical Benefits for Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Immunotherapy: A Promising Frontier in Prostate Cancer Treatment for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Omega-3 Fatty Acids: A Promising Approach to Prostate Health in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- CyberKnife: Advanced, Non-Invasive Prostate Cancer Treatment for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Alcohol Consumption and Prostate Health: Insights and Recommendations for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Proton Therapy: A Targeted Approach to Treating Prostate Cancer in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Targeted Therapy: Revolutionizing Prostate Cancer Treatment for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Stress Impact on Prostate Health: Management Strategies for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Heavy Metals and Prostate Health: Risks and Prevention Strategies for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Photodynamic Therapy: A Promising Treatment for Prostate Cancer in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hormone Therapy: Managing Prostate Cancer and Enhancing Life Quality [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Pesticides and Prostate Health: Risks, Mechanisms, and Prevention for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Green Tea Benefits for Prostate Health in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Antioxidants: Key to Prostate Health and Disease Prevention in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Selenium's Role in Prostate Health: Benefits and Optimal Intake for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Air Pollution's Emerging Link to Prostate Health Issues in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Lycopene's Role in Enhancing Prostate Health: Benefits and Dietary Sources [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Prostate Cancer Management: Understanding Watchful Waiting and Its Benefits [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Prostate and Bone Health: Understanding the Connection and Management Strategies [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Zinc's Vital Role in Prostate Health for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Plastics and Prostate Health: Risks, Research, and Mitigation Strategies for American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Chronic Inflammation's Impact on Prostate Health in American Males: Risks and Management [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Chemoprevention Strategies for Prostate Cancer: Agents and Clinical Insights [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Prostate Cancer Surgery: Benefits, Risks, and Comprehensive Management for American Men [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- EMFs and Prostate Health: Risks, Mechanisms, and Mitigation Strategies for American Males [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Vitamin E's Role in Prostate Health: Benefits and Considerations for American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Robotic Surgery for Prostate Cancer: Benefits and Procedure for American Men [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- Prostate Cancer: Focal Therapy's Role in Minimizing Side Effects for American Men [Last Updated On: April 3rd, 2025] [Originally Added On: April 3rd, 2025]
- Cruciferous Vegetables: A Dietary Approach to Enhancing Prostate Health in American Males [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Endocrine Disruptors and Prostate Health: Risks, Exposure, and Mitigation Strategies [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Industrial Chemicals and Prostate Health: Risks and Prevention Strategies [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Soy Benefits for Prostate Health: Reducing Cancer Risk and Managing BPH [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Laparoscopic Prostatectomy: Minimally Invasive Cancer Treatment and Recovery Insights [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Adjuvant Therapy's Role in Managing Prostate Cancer Among American Men [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Salvage Therapy: A Second Chance for American Men with Prostate Cancer Recurrence [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Neoadjuvant Therapy in Prostate Cancer: Insights for American Men's Health [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Medications and Prostate Health: Impacts, Monitoring, and Holistic Management for American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Flaxseed: A Natural Approach to Enhancing Prostate Health in American Males [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Pomegranates: A Natural Approach to Enhancing Prostate Health in American Males [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Palliative Surgery for Prostate Cancer: Enhancing Quality of Life for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Bisphosphonates: Enhancing Bone Health in Metastatic Prostate Cancer Management [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Shift Work's Impact on Prostate Health: Risks and Mitigation Strategies [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Ginger's Potential Benefits for Prostate Health in American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Radium-223: A Targeted Therapy for Advanced Prostate Cancer in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Heavy Physical Work's Impact on Prostate Health in American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Turmeric's Role in Enhancing Prostate Health: Benefits and Clinical Insights [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Abiraterone: Advancing Treatment for Metastatic Prostate Cancer in American Men [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Denosumab: A Promising Treatment for Prostate Cancer with Bone Metastases [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- RANK Ligand Inhibitors: A New Hope in Managing Advanced Prostate Cancer [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Prostate Health Risks and Strategies for Long-Haul Truckers [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Enzalutamide: A New Hope in Prostate Cancer Treatment for American Men [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Prostate Cancer: Symptoms, Diagnosis, Treatment, and Proactive Health for American Males [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
- Tomatoes and Prostate Health: The Role of Lycopene in Cancer Prevention [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
Word Count: 591