Introduction
Secondary hypogonadism, a condition characterized by the inadequate production of testosterone due to dysfunctions in the hypothalamus or pituitary gland, has been increasingly recognized not only as an endocrine disorder but also as having potential connections with other systemic health issues. Recent research has begun to explore the intricate relationship between secondary hypogonadism and gastrointestinal health, particularly in American males. This article delves into a prospective study that examines how digestive function might influence hormonal levels and contribute to the development of secondary hypogonadism.
Understanding Secondary Hypogonadism
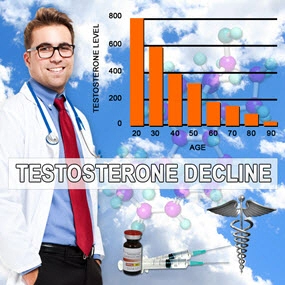
Secondary hypogonadism is distinct from primary hypogonadism, where the testes themselves fail to produce adequate testosterone. In secondary hypogonadism, the issue lies upstream in the hormonal cascade, with the hypothalamus and pituitary gland failing to stimulate the testes effectively. Symptoms can include decreased libido, erectile dysfunction, fatigue, and mood changes. While the condition is often linked to obesity, stress, and chronic illnesses, emerging evidence suggests a possible association with gastrointestinal health.
The Gastrointestinal-Hormonal Connection
The gastrointestinal tract plays a crucial role in overall health, including the absorption of nutrients necessary for hormone synthesis. The gut microbiome, in particular, has been identified as a key player in modulating systemic inflammation and metabolic processes, which can impact endocrine function. Dysbiosis, or an imbalance in gut bacteria, has been linked to various health conditions, including those affecting hormonal balance.
Study Design and Methodology
The prospective study in question involved a cohort of American males aged 30 to 60, selected to represent a broad demographic spectrum. Participants underwent comprehensive assessments of their gastrointestinal health, including stool analyses to evaluate the gut microbiome, and blood tests to measure testosterone and other hormone levels. Additionally, participants completed questionnaires regarding their digestive symptoms and overall health.
Key Findings
The study revealed a significant correlation between markers of poor gastrointestinal health and lower testosterone levels. Men with higher incidences of digestive issues, such as bloating, constipation, and diarrhea, were more likely to exhibit symptoms of secondary hypogonadism. Furthermore, those with dysbiosis showed a notable decrease in testosterone compared to those with a balanced gut microbiome.
Implications for Treatment and Management
These findings suggest that addressing gastrointestinal health could be a novel approach to managing secondary hypogonadism. Probiotics, dietary modifications, and other interventions aimed at improving gut health may help restore hormonal balance. Clinicians might consider integrating gastrointestinal assessments into the diagnostic and treatment protocols for men presenting with symptoms of secondary hypogonadism.
Challenges and Future Directions
While the study provides valuable insights, it is not without limitations. The sample size was relatively small, and further research with larger cohorts is needed to confirm these findings. Additionally, the exact mechanisms by which gastrointestinal health influences testosterone production remain to be fully elucidated. Future studies should aim to explore these pathways and identify specific interventions that could mitigate the risk of secondary hypogonadism through improved gut health.
Conclusion
The prospective study examining the association between secondary hypogonadism and gastrointestinal health in American males highlights a potentially significant link that warrants further investigation. As our understanding of the gut-hormone axis grows, so too does the potential for innovative treatment strategies that address both digestive and endocrine health. For American men struggling with secondary hypogonadism, this research opens new avenues for holistic care and improved quality of life.
Contact Us Today For A Free Consultation

- Secondary Hypogonadism: Impacts on Cardiovascular Health and Management Strategies [Last Updated On: February 25th, 2025] [Originally Added On: February 25th, 2025]
- Secondary Hypogonadism in American Men: Importance of Regular Check-ups for Early Detection and Management [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Genetic Insights into Secondary Hypogonadism in American Males: Diagnosis and Treatment [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Exercise Regimens for Managing Secondary Hypogonadism in American Males [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Secondary Hypogonadism's Impact on Sleep: Strategies for American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Stress-Induced Secondary Hypogonadism: Impact and Management Strategies for American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Secondary Hypogonadism: Impact on Energy and Treatment Options in American Males [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Secondary Hypogonadism's Impact on Body Composition in American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Managing Secondary Hypogonadism: Comprehensive Support for American Men's Health [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Secondary Hypogonadism: Impacts on Mental Health and Treatment Approaches in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism: Understanding Impacts and Managing Prostate Health in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Testing, and Treatment for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism: Impact on Immune System and Health in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism and Mood Disorders: Impact and Clinical Management in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism in American Males: Causes, Symptoms, and Treatment Options [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism and Diabetes: Prevalence, Link, and Management in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism and Hair Loss: Causes, Diagnosis, and Treatment Options for American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Exploring Alternative Therapies for Secondary Hypogonadism in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism in American Men: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism and Anemia: Causes, Symptoms, and Management in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Fat Distribution in American Men: Risks and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Kidney Function in American Males: Symptoms, Treatment, and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Causes, and Management Strategies for American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Secondary Hypogonadism in American Males: Diagnosis, Treatment, and Support [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism's Impact on Skin Health in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism: Key Nutrients and Dietary Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism: Understanding Its Profound Social Impact on American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism in American Males: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism's Impact on Bone Density in American Men: Diagnosis and Management [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Environmental Factors and Secondary Hypogonadism in American Men: Impacts and Interventions [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Lifestyle Impact on Secondary Hypogonadism in American Males: Prevention and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism and Fatigue: Diagnosis, Treatment, and Management for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Thyroid Function's Impact on Secondary Hypogonadism in American Males: Diagnosis and Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Impact on Libido and Health in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Sleep Disorders and Secondary Hypogonadism: Impact on American Men's Health [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Impacts on Health and Treatment Strategies for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism: Impacts, Mental Health Needs, and Integrated Care Solutions for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism's Psychological Impact on American Men: A Comprehensive Overview [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Secondary Hypogonadism: Stress, Strategies, and Support for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism and Autoimmune Diseases: A Rising Concern in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Exercise Boosts Testosterone and Alleviates Secondary Hypogonadism Symptoms in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism's Impact on Emotional Well-being in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism and Liver Health: Impacts and Management in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism: Impacts on Physical Performance and Management Strategies [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism and Cardiovascular Risks in American Males: A Comprehensive Overview [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism's Impact on Muscle Strength in American Men: Diagnosis and Treatment [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism in American Males: Symptoms, Monitoring, and Management Strategies [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism: Impact on Mood and Treatment in American Men [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Secondary Hypogonadism: Causes, Symptoms, and Comprehensive Management Strategies [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Managing Secondary Hypogonadism: Diagnosis, Hormonal Therapy, and Lifestyle Strategies for American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Secondary Hypogonadism: Impact on Energy, Vitality, and Treatment Options for American Men [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Secondary Hypogonadism in American Males: Weight Management and Holistic Health Strategies [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Managing Secondary Hypogonadism: The Crucial Role of Diet and Nutrients [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Managing Secondary Hypogonadism: Diagnosis, Treatment, and Enhancing Quality of Life [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Secondary Hypogonadism: Impacts on Men's Relationships and Management Strategies [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Secondary Hypogonadism in American Males: The Critical Impact of Sleep Deprivation [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Secondary Hypogonadism: A Holistic Approach for American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Secondary Hypogonadism's Impact on Mental Clarity in American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Community Support's Vital Role in Managing Secondary Hypogonadism in American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Secondary Hypogonadism's Impact on Emotional Resilience in American Men [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Managing Secondary Hypogonadism: A Holistic Approach for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Understanding and Managing Secondary Hypogonadism in American Males [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Secondary Hypogonadism in American Males: Diagnosis, Treatment, and Personalized Care [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Secondary Hypogonadism's Impact on Mental Health in American Males: Diagnosis and Treatment [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Understanding Secondary Hypogonadism: Causes, Symptoms, and Management for American Males [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Causes, and Management Strategies for American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Secondary Hypogonadism: Impacts on Muscle, Bone, and Cardiovascular Health in American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Secondary Hypogonadism's Impact on Self-Esteem in American Men: Causes and Management [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Understanding, Diagnosing, and Enhancing Vitality in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Understanding Causes, Symptoms, and Management in American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Importance of Regular Health Check-ups for American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Lifestyle Factors and Secondary Hypogonadism: Impacts and Prevention Strategies for American Males [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Secondary Hypogonadism: Emotional Impact and Comprehensive Management in American Men [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Secondary Hypogonadism in American Men: Symptoms, Impacts, and Management Strategies [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
- Secondary Hypogonadism: Impacts on Health and Importance of Early Detection in Men [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
Word Count: 542