Introduction
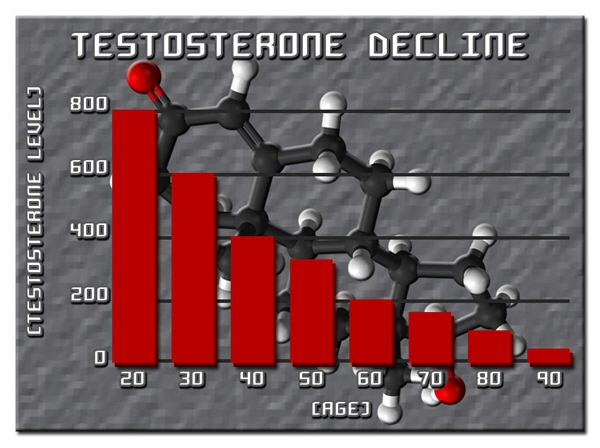
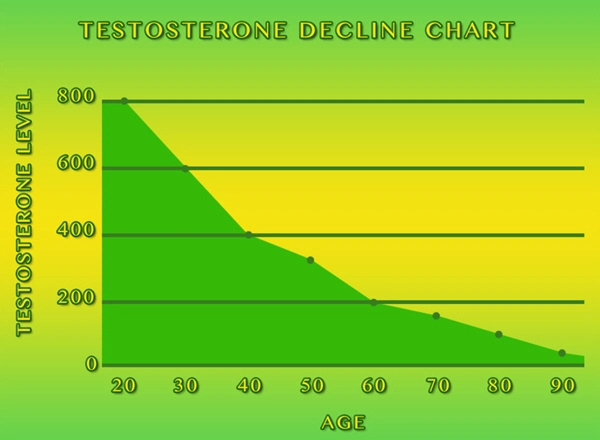
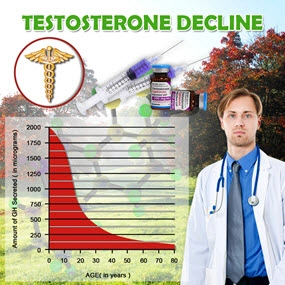
Secondary hypogonadism, a condition characterized by the inadequate production of testosterone due to dysfunctions in the hypothalamus or pituitary gland, has been increasingly recognized as a significant health concern among American males. This condition not only affects sexual and reproductive functions but also has broader implications on metabolic health, particularly lipid profiles and cardiovascular risk. This article delves into the clinical and laboratory data that elucidate the effects of secondary hypogonadism on these critical health parameters, aiming to provide a comprehensive understanding for healthcare professionals and patients alike.
Understanding Secondary Hypogonadism
Secondary hypogonadism results from a disruption in the hypothalamic-pituitary-gonadal axis, which can be caused by various factors including tumors, genetic conditions, and chronic illnesses. Unlike primary hypogonadism, which stems from testicular failure, secondary hypogonadism is characterized by low or inappropriately normal gonadotropin levels alongside decreased testosterone production. This hormonal imbalance can have far-reaching effects beyond reproductive health.
Effects on Lipid Profiles
Numerous studies have established a link between low testosterone levels and adverse changes in lipid profiles. Specifically, men with secondary hypogonadism often exhibit elevated levels of total cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides, alongside reduced levels of high-density lipoprotein (HDL) cholesterol. These alterations in lipid metabolism are significant because they are well-established risk factors for atherosclerosis and subsequent cardiovascular disease. The mechanism behind these changes is thought to involve testosterone's influence on hepatic lipase activity and adipocyte function, which in turn affects lipid synthesis and clearance.
Cardiovascular Risk and Secondary Hypogonadism
The relationship between secondary hypogonadism and cardiovascular risk is complex and multifaceted. Beyond the direct impact on lipid profiles, low testosterone levels have been associated with increased visceral adiposity, insulin resistance, and systemic inflammation—all of which are known contributors to cardiovascular disease. Additionally, testosterone deficiency may lead to endothelial dysfunction, a precursor to atherosclerosis. Clinical data suggest that men with secondary hypogonadism have a higher prevalence of cardiovascular events, including myocardial infarction and stroke, compared to their eugonadal counterparts.
Clinical and Laboratory Data
A review of clinical trials and observational studies provides compelling evidence of the association between secondary hypogonadism and adverse cardiovascular outcomes. For instance, a longitudinal study involving American males with secondary hypogonadism demonstrated a significant correlation between low testosterone levels and increased carotid intima-media thickness, a marker of subclinical atherosclerosis. Similarly, laboratory data from these studies consistently show a detrimental shift in lipid profiles among affected individuals, underscoring the need for targeted interventions.
Management and Treatment Considerations
Given the cardiovascular implications of secondary hypogonadism, effective management strategies are crucial. Testosterone replacement therapy (TRT) has been shown to improve lipid profiles and reduce cardiovascular risk in some studies, although its use must be carefully considered due to potential side effects and the need for long-term monitoring. Lifestyle modifications, including diet and exercise, also play a vital role in mitigating the metabolic effects of low testosterone levels. Healthcare providers should adopt a holistic approach, addressing both the hormonal and cardiovascular aspects of the condition.
Conclusion
Secondary hypogonadism represents a significant health challenge for American males, with profound implications for lipid profiles and cardiovascular risk. The clinical and laboratory data reviewed herein underscore the importance of early detection and comprehensive management of this condition. By understanding the intricate relationship between testosterone deficiency and cardiovascular health, healthcare professionals can better tailor interventions to improve patient outcomes and quality of life. As research continues to evolve, it is imperative that the medical community remains vigilant in addressing the multifaceted impacts of secondary hypogonadism on men's health.
Contact Us Today For A Free Consultation

- Secondary Hypogonadism: Impacts on Cardiovascular Health and Management Strategies [Last Updated On: February 25th, 2025] [Originally Added On: February 25th, 2025]
- Secondary Hypogonadism in American Men: Importance of Regular Check-ups for Early Detection and Management [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Genetic Insights into Secondary Hypogonadism in American Males: Diagnosis and Treatment [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Exercise Regimens for Managing Secondary Hypogonadism in American Males [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Secondary Hypogonadism's Impact on Sleep: Strategies for American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Stress-Induced Secondary Hypogonadism: Impact and Management Strategies for American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Secondary Hypogonadism: Impact on Energy and Treatment Options in American Males [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Secondary Hypogonadism's Impact on Body Composition in American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Managing Secondary Hypogonadism: Comprehensive Support for American Men's Health [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Secondary Hypogonadism: Impacts on Mental Health and Treatment Approaches in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism: Understanding Impacts and Managing Prostate Health in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Testing, and Treatment for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism: Impact on Immune System and Health in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism and Mood Disorders: Impact and Clinical Management in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism in American Males: Causes, Symptoms, and Treatment Options [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism and Diabetes: Prevalence, Link, and Management in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism and Hair Loss: Causes, Diagnosis, and Treatment Options for American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Exploring Alternative Therapies for Secondary Hypogonadism in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism in American Men: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism and Anemia: Causes, Symptoms, and Management in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Fat Distribution in American Men: Risks and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Kidney Function in American Males: Symptoms, Treatment, and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Causes, and Management Strategies for American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Managing Secondary Hypogonadism in American Males: Diagnosis, Treatment, and Support [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism's Impact on Skin Health in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism: Key Nutrients and Dietary Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism: Understanding Its Profound Social Impact on American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism in American Males: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism's Impact on Bone Density in American Men: Diagnosis and Management [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Environmental Factors and Secondary Hypogonadism in American Men: Impacts and Interventions [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Lifestyle Impact on Secondary Hypogonadism in American Males: Prevention and Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism and Fatigue: Diagnosis, Treatment, and Management for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Thyroid Function's Impact on Secondary Hypogonadism in American Males: Diagnosis and Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Impact on Libido and Health in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Sleep Disorders and Secondary Hypogonadism: Impact on American Men's Health [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Impacts on Health and Treatment Strategies for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism: Impacts, Mental Health Needs, and Integrated Care Solutions for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism's Psychological Impact on American Men: A Comprehensive Overview [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Secondary Hypogonadism: Stress, Strategies, and Support for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism and Autoimmune Diseases: A Rising Concern in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Exercise Boosts Testosterone and Alleviates Secondary Hypogonadism Symptoms in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism's Impact on Emotional Well-being in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism and Liver Health: Impacts and Management in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism: Impacts on Physical Performance and Management Strategies [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism and Cardiovascular Risks in American Males: A Comprehensive Overview [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Secondary Hypogonadism's Impact on Muscle Strength in American Men: Diagnosis and Treatment [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism in American Males: Symptoms, Monitoring, and Management Strategies [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism: Impact on Mood and Treatment in American Men [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Secondary Hypogonadism: Causes, Symptoms, and Comprehensive Management Strategies [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Managing Secondary Hypogonadism: Diagnosis, Hormonal Therapy, and Lifestyle Strategies for American Males [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- Secondary Hypogonadism: Impact on Energy, Vitality, and Treatment Options for American Men [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Secondary Hypogonadism in American Males: Weight Management and Holistic Health Strategies [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Managing Secondary Hypogonadism: The Crucial Role of Diet and Nutrients [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Managing Secondary Hypogonadism: Diagnosis, Treatment, and Enhancing Quality of Life [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Secondary Hypogonadism: Impacts on Men's Relationships and Management Strategies [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Secondary Hypogonadism in American Males: The Critical Impact of Sleep Deprivation [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Managing Secondary Hypogonadism: A Holistic Approach for American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Secondary Hypogonadism's Impact on Mental Clarity in American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Community Support's Vital Role in Managing Secondary Hypogonadism in American Men [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Secondary Hypogonadism's Impact on Emotional Resilience in American Men [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Managing Secondary Hypogonadism: A Holistic Approach for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Understanding and Managing Secondary Hypogonadism in American Males [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Secondary Hypogonadism in American Males: Diagnosis, Treatment, and Personalized Care [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Secondary Hypogonadism's Impact on Mental Health in American Males: Diagnosis and Treatment [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Understanding Secondary Hypogonadism: Causes, Symptoms, and Management for American Males [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Causes, and Management Strategies for American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Secondary Hypogonadism: Impacts on Muscle, Bone, and Cardiovascular Health in American Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Secondary Hypogonadism's Impact on Self-Esteem in American Men: Causes and Management [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Understanding, Diagnosing, and Enhancing Vitality in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism in American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Understanding Causes, Symptoms, and Management in American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Importance of Regular Health Check-ups for American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Lifestyle Factors and Secondary Hypogonadism: Impacts and Prevention Strategies for American Males [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- Secondary Hypogonadism: Emotional Impact and Comprehensive Management in American Men [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Secondary Hypogonadism in American Men: Symptoms, Impacts, and Management Strategies [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
- Secondary Hypogonadism: Impacts on Health and Importance of Early Detection in Men [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
Word Count: 580